Why People Are Rethinking Flagyl for Bacterial Vaginosis
When you talk about treating bacterial vaginosis (BV), Flagyl—also called metronidazole—used to be the king. It’s been the go-to antibiotic for decades, both as a pill and a vaginal gel. But if you’ve ever taken it, you probably remember the metallic taste that won’t quit and the very real, very annoying nausea. Worst part? Recurrence rates can be as high as 50% within just six months after treatment, which leaves a lot of people frustrated and looking for alternatives to Flagyl.
Let’s get real: not everyone can even take Flagyl. People with allergies, folks who react badly to it, or those who’d rather avoid unpleasant side effects start searching for something better. And in 2025, medicine finally caught up to that need. The medical world isn’t pushing just one answer anymore—new options have hit the scene, and some old ones have proven they can hold their own. If you want a crystal-clear look at what’s out there, you’re in the right place.
To save you the same painful, hours-long research rabbit holes, we’ll dive into secnidazole (the newer kid on the block), clindamycin (an old favourite making a comeback in new forms), and probiotics (which are finally getting more proven respect). New guidelines and real-world stories from patients right here in Australia show things are changing. Keep an open mind—you might find your doctor visits look different this year.

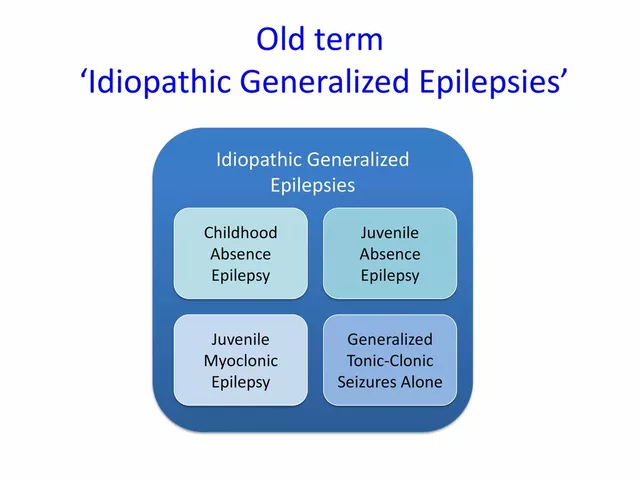
Secnidazole and Clindamycin: Comparing New and Old Antibiotic Champs
Secnidazole is pretty new in Australia as a BV treatment. It’s actually part of the same drug family as Flagyl but with big, practical differences. Instead of taking pills twice a day for a week, secnidazole lets patients take just one, big dose. This one-and-done style is a real winner for people who struggle with sticking to long treatment schedules or who can’t stand those classic antibiotic side effects day after day. The convenience is huge, especially if you’re juggling work, kids, or uni.
Because it has a longer half-life in your body, secnidazole keeps working long after you swallow it, giving those bad bacteria less chance for a comeback. Of course, every drug has its own baggage—side effects are mostly mild, like headache or nausea, but they tend to not last as long since the course is so quick. In 2024, several women I spoke with swapped to secnidazole after multiple failed rounds of Flagyl, and most reported fewer recurrences and a much easier experience. A 2023 clinical review in "The Australian Journal of General Practice" even listed secnidazole as potentially matching or outperforming Flagyl for recurrence and symptom relief rates.
Switching gears to clindamycin, you’ll see it’s been in the mix for decades, mainly as a backup when Flagyl fails. But modern clindamycin vaginal creams and ovules have made it easier to get high concentrations of the medication precisely where it’s needed, without blitzing your whole gut microbiome with yet another round of oral antibiotics. Less impact on the stomach, fewer headaches, and directly targeting BV—what’s not to love? The only big downside: be cautious if you’re breastfeeding or have a history of gut issues, like colitis, as clindamycin can sometimes disturb bowel flora and cause upset. For many, though, it’s now considered a first-line therapy, especially for recurring BV or that stubborn case that won’t quit.
One tip? Ask your doctor about the vaginal version first, then try the oral form if you really need it. Here’s a snapshot to help compare:
| Treatment | Typical Dosage | Main Side Effects | Recurrence Rate (6mo) |
|---|---|---|---|
| Flagyl (metronidazole) | Twice daily x 7 days | Nausea, headache, metallic taste | 40-50% |
| Secnidazole | Single dose | Transient nausea/headache | 30-35% |
| Clindamycin | Vaginal cream 7 days/ oral tabs | Vaginal irritation, GI upset | 25-40% |
If you want a deep dive on all the new and upcoming treatments (including several not in this article), check out this detailed resource on alternatives to Flagyl. It’s worth keeping handy if your current medication isn’t getting the job done, or you’re worried about antibiotic resistance.

Probiotics and Real Lifestyle Strategies: Science Backs the Hype in 2025
Doctors used to roll their eyes whenever anyone mentioned probiotics for BV. Fast-forward to 2025, and now they’re often part of a dual-therapy approach—especially for stubborn, recurring cases. The reason? BV is all about a disturbed vaginal microbiome, where good bacteria like Lactobacillus plummet and harmful ones take over. If you only nuke the bad with antibiotics, you’re left with a sort of microbial “blank slate” that bad ones can recolonize, quickly. But if you actively help the good bacteria grow back, either by taking probiotics or using them intravaginally, the relapse rates drop.
Not all probiotics are created equal, though. Only a handful of strains have real research behind them—mainly the ones in the Lactobacillus family, especially L. crispatus and L. rhamnosus. Some 2024 local studies out of Melbourne actually tracked women using a probiotic vaginal suppository after antibiotics, and the recurrence rate at six months dropped from about 40% to 20%. That’s massive! Plenty of over-the-counter products in Australia now offer these specific strains, just make sure the label spells them out and that there’s a viable amount (usually at least 1 billion CFU per dose).
Taking probiotics orally helps, but for really tough cases (like if you’ve had BV three or more times in a year), the vaginal approach is winning the science race. This means tiny dissolvable tablets or gels—messy, maybe, but effective. Discuss with your GP or women’s health clinic for legit options you can grab without needing an expensive compounding pharmacy.
There’s also some cool new research using wearable vaginal sensors (kind of wild, right?) to measure pH and microbiome changes in real time. These are rolling out in clinical trials across New South Wales this year, and they might end up as take-home tools—letting people spot BV recurrences way earlier and treat them before symptoms get out of control. Imagine never having to panic mid-date about a sudden flare-up again.
Practical lifestyle tweaks still make a difference. Things like wearing breathable cotton underwear, avoiding douching (seriously, it wipes out good bacteria), and gentle hygiene products cut irritations and make relapses less likely. One fun fact: people who eat a diet rich in prebiotics—fibres that feed good bacteria, like those found in bananas, garlic, oats, and asparagus—may keep their vaginal microbiome more stable. This isn’t magic, but it can boost whatever medical therapy you’re on.
If you’re weighing your options, remember: the best treatment is the one that keeps you symptom-free without tossing your life upside down. Some people swear by probiotics alone, especially if they’re in the “mild but recurring” camp, while others need a stronger, two-pronged attack with new antibiotics plus microbiome support. And if you’re not sure what’s right for you, it helps to talk to a doctor, nurse, or pharmacist who’s up to speed on the newest research—not just the old school, “just take Flagyl again” script.
Stick with what works, but don’t be afraid to ask about the newest—and best tested—alternatives to Flagyl. Whether it’s a single-dose secnidazole, a smart use of clindamycin, or giving probiotics a real shot, the options for beating BV are a lot better in 2025 than they were just a few years ago. You’re not stuck with just one answer anymore, and your comfort actually matters.



Mina Berens
July 18, 2025 at 11:31
Oh wow, this is super helpful! 😍 I’ve always just heard about Flagyl but never knew there were other legit options like secnidazole and probiotics. It's kinda comforting to know there are alternatives, especially for folks whose bodies react badly to one type of medication.
Also, clindamycin sounds interesting—I wonder how it compares in terms of side effects? The inclusion of probiotics feels so refreshing because sometimes natural options or supplements can really assist alongside meds.
Would love to see some personal experiences or maybe tips on how long someone should expect to be on each treatment. Thanks for sharing this clear info!