It starts with a simple course of antibiotics. Maybe it was for a sinus infection, a urinary tract infection, or even a dental procedure. You take the pills as directed, feel better, and move on. But days or weeks later, the diarrhea hits-persistent, watery, sometimes bloody. Then comes the cramps, the fever, the exhaustion. You go back to the doctor, and they say: C. difficile. Not just any stomach bug. This is a dangerous, often recurrent infection that can turn deadly if ignored.
Why Antibiotics Are the Main Culprit
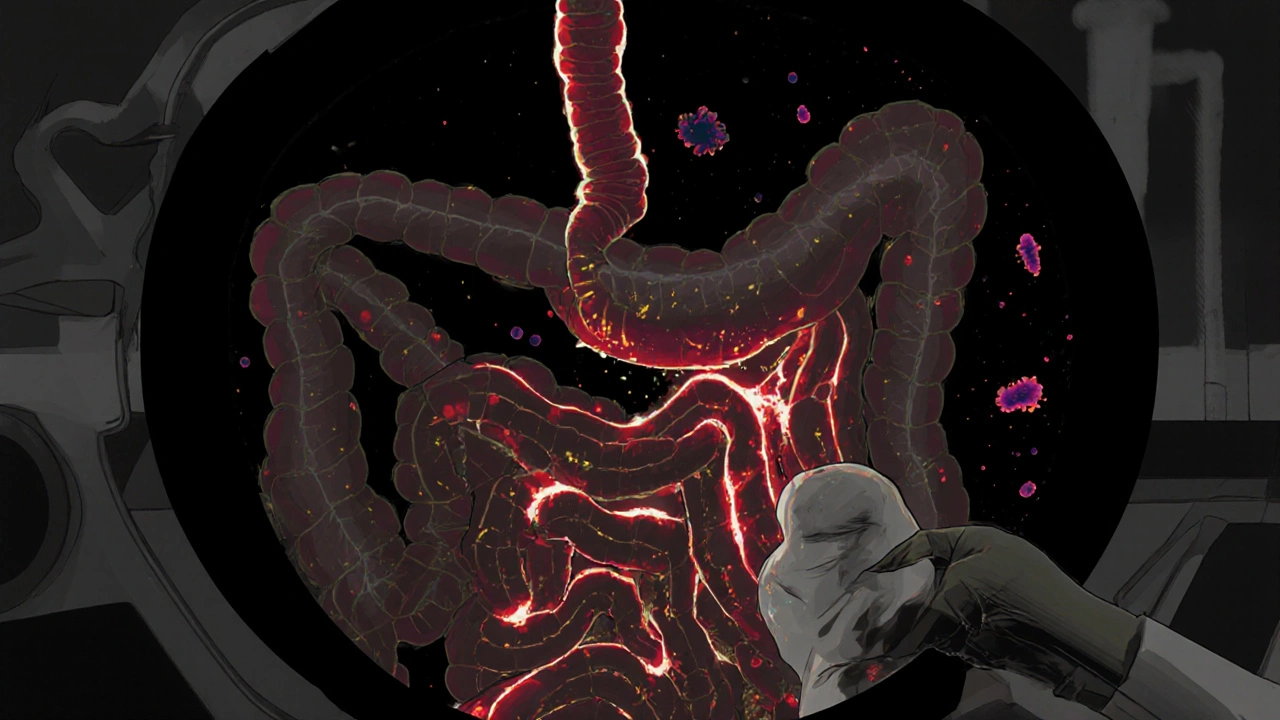
Your gut is full of bacteria. Trillions of them. Most are harmless. Some are helpful. They digest food, train your immune system, and keep bad actors in check. But when you take antibiotics-especially broad-spectrum ones-you don’t just kill the bad bacteria. You wipe out the good ones too. And that’s when Clostridioides difficile, or C. diff, gets its chance.It’s not that antibiotics cause C. diff. They don’t. The bacteria are already there, lying low in your gut, waiting. About 5% of healthy adults carry it without symptoms. But when your microbiome gets thrown off balance, C. diff multiplies like wildfire. It releases toxins that eat away at your colon lining. That’s what causes the severe diarrhea, inflammation, and sometimes life-threatening complications like toxic megacolon or colon rupture.
Not all antibiotics are created equal when it comes to risk. Some are far more likely to trigger C. diff than others. Studies show clindamycin, later-generation cephalosporins like ceftriaxone, and fluoroquinolones like ciprofloxacin carry the highest risk. But the biggest offender? Piperacillin-tazobactam-a common hospital antibiotic. Research from 2023 found it nearly doubles the risk of C. diff compared to other drugs. Each extra day on antibiotics increases your risk by 8%. And it’s not just the length-it’s the timing. Risk spikes after 14 days of use, then stays high.
Even more concerning: community-acquired C. diff is rising. People who never set foot in a hospital are getting it. Why? Because they took an antibiotic for a cold, a sore throat, or a minor infection that didn’t need one in the first place. A 2023 NIH study found nearly half of community C. diff cases happened within 30 days of antibiotic use. The CDC calls this an urgent threat. In the U.S. alone, there are 500,000 cases every year, and 29,000 people die from it.
What Happens When Standard Treatment Fails
The first-line treatment for C. diff is usually vancomycin or fidaxomicin. Both work-sometimes. But here’s the problem: up to 30% of patients come back with another infection after finishing the course. And once you’ve had one recurrence, your chances of another jump to 60%. After three or more recurrences, the odds of another flare-up are over 80%.Why does this keep happening? Because the antibiotics kill the C. diff-but they don’t fix your gut. The microbiome stays broken. The good bacteria haven’t returned. So the C. diff spores, which are tough as nails, just wait for another chance to grow.
Doctors often try the same antibiotic again. Or switch to a different one. Sometimes they add probiotics. But the evidence for probiotics is weak-and in some cases, dangerous. The IDSA says there’s not enough proof they prevent C. diff, and in immunocompromised people, they’ve been linked to bloodstream infections. So what’s left?
Fecal Transplants: The Unexpected Cure
Enter fecal microbiota transplantation, or FMT. It sounds extreme. And it is. But it’s also one of the most effective treatments in modern medicine for recurrent C. diff.In 2013, a landmark study in the New England Journal of Medicine compared FMT to standard antibiotic treatment for recurrent C. diff. The results were shocking. After one treatment, 81% of FMT patients were cured. After a second treatment, 94% were cured. The antibiotic group? Only 31% got better. That’s not a slight edge. That’s a revolution.
The procedure is simple in concept: take healthy stool from a carefully screened donor, mix it with saline, and deliver it into the patient’s colon. It’s not about the poop itself-it’s about the bacteria inside it. These good microbes outcompete C. diff, restore balance, and shut down the infection.
Today, FMT is recommended by the American Gastroenterological Association for anyone who’s had three or more recurrences. Success rates? 85% to 90%. That’s better than most cancer treatments. And it’s not just for hospitals anymore. The FDA approved two standardized FMT products in 2022 and 2023-Rebyota and Vowst-delivered as oral capsules. No colonoscopy needed. Just swallow a pill.
Delivery methods vary. About 65% of FMTs are done via colonoscopy. Another 20% use enemas. The rest are capsules. All are effective. The key is donor screening. Donors are tested for HIV, hepatitis, parasites, and even antibiotic-resistant bacteria. One wrong stool sample could introduce a new threat. That’s why you don’t get this from a friend’s basement.
Who Benefits Most from FMT?
FMT isn’t for everyone. It’s not the first line of defense. It’s the last resort-for people who’ve tried everything else and keep coming back. But for those people, it’s life-changing.One patient from Sydney, who asked to remain anonymous, had five recurrences over 18 months. Each time, she was hospitalized. Each time, she was put on vancomycin. Each time, it worked-until it didn’t. She lost weight. She couldn’t work. She stopped seeing friends. After her fifth relapse, her gastroenterologist suggested FMT. She was terrified. But she did it. Within days, her symptoms vanished. Six months later, she’s back to hiking, cooking, and traveling. No more antibiotics. No more fear.
That’s the pattern. People who’ve suffered through multiple recurrences often describe FMT as a second chance. The CDC estimates that each hospitalization for C. diff costs $11,000. FMT? Around $2,000. That’s not just better health-it’s better economics.
What Comes After FMT?
FMT isn’t the end of the story. It’s a bridge. Researchers are now working on the next generation of microbiome therapies. SER-109, an oral pill made from purified bacterial spores, showed 88% success in a major 2022 trial. It’s cleaner, more precise, and doesn’t involve stool at all. Companies are developing targeted probiotics, monoclonal antibodies, and even engineered bacteria that specifically attack C. diff without harming the rest of the gut.Meanwhile, prevention is still the best strategy. Antibiotic stewardship matters. Doctors are being trained to ask: Do you really need this antibiotic? Can we use something narrower? Can we shorten the course? The NICE guidelines say: review antibiotics within 48 to 72 hours. If it’s not helping, stop it.
And for people who’ve had C. diff before? Avoid unnecessary antibiotics. If you’re going into the hospital, ask if they’re using infection control protocols. Wash your hands with soap and water-alcohol gels don’t kill C. diff spores. And if you’re on antibiotics and start having diarrhea, don’t wait. Get tested early.
Why This Matters Beyond the Individual
C. diff isn’t just a personal health problem. It’s a public health crisis. Hospitals spend billions treating it. Communities are seeing more cases. And the bacteria are evolving. The fluoroquinolone-resistant ribotype 027 strain is spreading outside hospitals, making it harder to control.But there’s hope. FMT proved that fixing the microbiome works. That’s changed how we think about infections. We’re moving from killing bacteria to restoring balance. And that shift is already saving lives.
Next time you’re prescribed an antibiotic, ask: Is this necessary? Is there a safer option? And if you’ve had C. diff before? Know your options. FMT isn’t a last resort-it’s a lifeline.
Can you get C. difficile from someone else?
Yes. C. diff spreads through spores in feces. If someone with the infection doesn’t wash their hands properly, they can contaminate surfaces like doorknobs, toilets, or medical equipment. Others can pick up the spores and ingest them. That’s why handwashing with soap and water (not hand sanitizer) is critical in hospitals and homes. Asymptomatic carriers-people who have the bacteria but no symptoms-can also spread it, which makes outbreaks harder to stop.
Is fecal transplant safe?
When done through approved medical channels, FMT is very safe. Donors are rigorously screened for infections like HIV, hepatitis, and antibiotic-resistant bacteria. The FDA requires informed consent because there’s a small risk of introducing unknown pathogens or triggering long-term changes in the microbiome. Serious side effects are rare, but there have been cases of bacterial infections linked to unscreened stool. That’s why you should never try a DIY version. Only use FDA-approved products or procedures done in licensed clinics.
Do probiotics help prevent C. difficile?
Not reliably. Some studies show a small benefit, but major health organizations like the IDSA say there’s not enough proof to recommend them for prevention. Worse, in people with weakened immune systems, probiotics have been linked to serious infections like bloodstream infections. Don’t rely on yogurt or over-the-counter pills to protect you. The best protection is avoiding unnecessary antibiotics and practicing good hygiene.
How long does it take to recover after a fecal transplant?
Most people notice improvement within 24 to 48 hours. Diarrhea slows down, cramps ease, and energy returns. Full recovery-meaning no more symptoms and a stable microbiome-usually takes a few weeks. Some patients report feeling better than they have in years. Long-term follow-up studies show most people stay symptom-free for over a year, and many never have another episode.
Can C. difficile come back after FMT?
Yes, but it’s uncommon. About 10% to 15% of patients have a recurrence after FMT. That’s much lower than the 60%+ recurrence rate after antibiotics alone. If it does return, doctors may repeat the FMT or try newer therapies like SER-109. The key is avoiding another round of broad-spectrum antibiotics. Once your microbiome is restored, protecting it is just as important as fixing it.
Are there alternatives to fecal transplant?
Yes, but they’re less effective. For first-time infections, fidaxomicin is better than vancomycin at preventing recurrence. Bezlotoxumab, a monoclonal antibody given with antibiotics, reduces recurrence by 10%. But neither fixes the broken microbiome like FMT does. New oral therapies like SER-109 are showing promise and may replace FMT in the future. But for now, FMT remains the gold standard for recurrent cases.





shreyas yashas
November 22, 2025 at 11:03
Man, I never thought about how antibiotics wipe out the good guys too. I took cipro for a UTI last year and ended up with nasty diarrhea for weeks. No one warned me. Now I ask my doctor if it's really necessary before I take anything.