If you’ve ever felt that burning sensation rising from your stomach into your chest-especially after eating or lying down-you’re not alone. About 20% of adults in the U.S. deal with GERD symptoms at least once a week. For many, it’s more than just discomfort. It’s sleepless nights, constant throat clearing, or even a chronic cough that won’t go away. The good news? You don’t have to live with it. The best approach isn’t just popping pills-it’s combining smart lifestyle changes with the right medication, when needed.
What Really Happens in GERD?
GERD isn’t just occasional heartburn. It’s a chronic condition where the lower esophageal sphincter (LES)-a muscular ring between your stomach and esophagus-doesn’t close properly. This lets stomach acid, which can be as strong as pH 1.5, splash back up into your esophagus. Unlike your stomach, your esophagus doesn’t have a thick mucus lining to protect it. So when acid hits it regularly, it causes inflammation, pain, and sometimes long-term damage.Most people with GERD report heartburn (90% do), but others notice a sour taste in their mouth, hoarseness, or a persistent cough. These symptoms often get worse after eating fatty or spicy food, drinking coffee or alcohol, or lying down too soon after a meal. Studies show that if your esophagus is exposed to acid more than 5% of the time over 24 hours, it’s considered pathological GERD.
Some factors make GERD more likely. Obesity increases your risk by 2.5 times. A hiatal hernia-where part of the stomach pushes up through the diaphragm-is found in 94% of people with erosive esophagitis. Smoking doubles your chances. Even pregnancy can trigger it, affecting 30-50% of expectant mothers.
Why PPIs Are the Go-To Medication
When lifestyle changes alone aren’t enough, doctors turn to proton pump inhibitors (PPIs). These include omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix). Unlike antacids that just neutralize acid temporarily, or H2 blockers like famotidine that reduce acid by about 60-70%, PPIs cut acid production by 90-98%. They work by blocking the final step acid-producing cells in your stomach use to make acid.For people with visible damage to the esophagus (erosive esophagitis), PPIs heal the tissue in 70-90% of cases. That’s significantly better than H2 blockers, which heal only about half as often. Most people feel better within a few days, but full healing can take 4-8 weeks. That’s why doctors recommend taking them 30-60 minutes before your first meal-so they’re active when your stomach starts producing acid for digestion.
PPIs aren’t magic. They don’t fix the broken valve. They just turn down the acid. That’s why many people rely on them long-term. But here’s the catch: long-term use comes with risks.
The Hidden Costs of Long-Term PPI Use
Many patients stay on PPIs for years-even decades-without ever checking if they still need them. That’s a problem. Studies show that using PPIs for more than a year increases your risk of:- Enteric infections like Clostridium difficile (by 20-50%)
- Vitamin B12 deficiency (due to reduced stomach acid needed for absorption)
- Acute interstitial nephritis (a type of kidney inflammation)
- Higher risk of hip fractures in older adults (35% increased risk with use over 3 years)
The FDA has issued warnings on all these risks. And yet, about 15% of GERD patients take PPIs long-term, even though guidelines say to reevaluate use every 8 weeks. One study found that up to 70% of PPI prescriptions are unnecessary.
Another issue: rebound acid hypersecretion. When people stop PPIs suddenly, their stomach overcompensates by making even more acid than before. This can make symptoms worse for weeks. That’s why quitting PPIs isn’t as simple as just skipping a dose. You need to taper off slowly-often by switching to an H2 blocker first, then reducing that over 4-8 weeks.

Lifestyle Changes: The Real Game-Changer
The American College of Gastroenterology says lifestyle changes should be the first step for everyone with GERD. And they work. Losing just 5-10% of your body weight cuts symptoms by about 50%. That’s not a small win-it’s often enough to stop needing medication entirely.Here’s what actually helps, based on real patient data:
- Avoid eating 2-3 hours before bed. This reduces nighttime acid exposure by 40-60%. Elevating the head of your bed by 6 inches helps too-gravity keeps acid down.
- Eliminate trigger foods. Coffee, tomatoes, alcohol, chocolate, and fatty or spicy foods cause flare-ups in 70-80% of people. Cutting out just coffee helps 73% of users. Spicy foods? 68% report improvement.
- Stop smoking. Smoking relaxes the LES and reduces saliva production (which naturally neutralizes acid).
- Wear loose clothing. Tight belts or pants increase abdominal pressure, pushing stomach contents upward.
One patient in Sydney shared that after years of PPIs, he started tracking his meals with a free app called RefluxMD. He discovered that even though he avoided coffee, his evening yogurt with fruit triggered him. Once he swapped it for plain oats, his nighttime symptoms vanished.
Why Lifestyle Changes Are Hard to Stick With
The problem isn’t knowing what to do-it’s doing it consistently. A Cleveland Clinic survey found that 41% of patients struggle to maintain dietary changes because of social pressure, family meals, or cultural habits. You can’t avoid birthday cake at your kid’s party. You can’t say no to wine at dinner with friends every week.That’s why success isn’t about perfection. It’s about balance. You don’t have to give up everything. Try this: identify your top 3 triggers and eliminate them for 3 weeks. If your symptoms drop, you’ve found your personal list. Then, allow yourself occasional treats-but plan for them. Eat earlier. Take an antacid beforehand. Stay upright afterward.
Many people find that once they start feeling better, they’re more motivated to keep going. The energy boost from sleeping through the night? The relief from not needing to carry antacids everywhere? Those are powerful reinforcers.
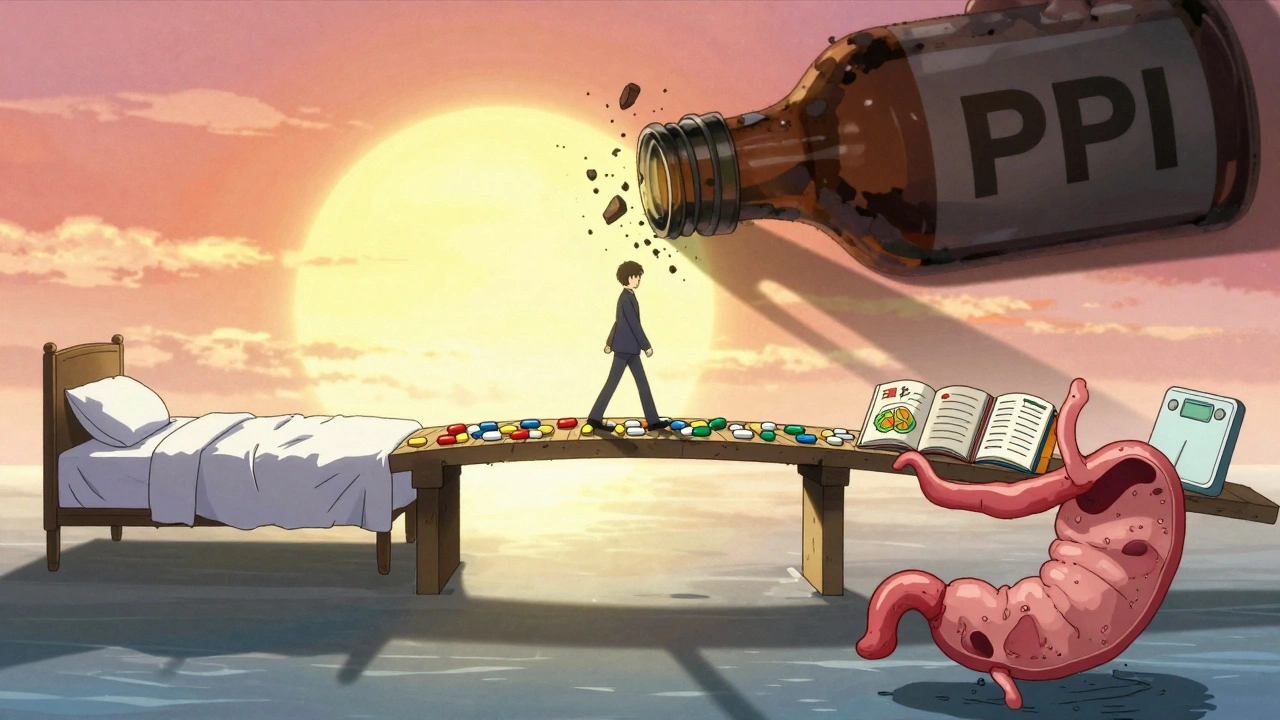
When Medication and Lifestyle Work Together
The best outcomes happen when people use PPIs as a bridge-not a lifeline. Start with lifestyle changes for 2-4 weeks. If symptoms persist, add a low-dose PPI. Once symptoms improve, try to taper off the PPI while keeping the lifestyle habits. A 2023 Johns Hopkins study showed that a structured 12-week program combining diet, weight loss, and sleep adjustments allowed 65% of patients to stop PPIs entirely-without symptoms returning.For those who still need medication after lifestyle changes, don’t assume you’re stuck. Ask your doctor about:
- Switching to an H2 blocker for maintenance
- Using PPIs only on-demand (e.g., before a big meal)
- Trying the newer drug vonoprazan (Voquezna), approved in 2023, which works faster and may have fewer long-term risks than PPIs
And if you’ve had GERD for more than 5 years, especially with ongoing symptoms despite treatment, get an endoscopy. That’s the only way to check for Barrett’s esophagus-a precancerous condition that develops in 10-15% of long-term GERD patients.
What to Do If Nothing Seems to Work
If you’ve tried lifestyle changes, taken PPIs for months, and still have symptoms, it’s time to dig deeper. Ask your doctor about:- Non-acid reflux (bile or gas can cause similar symptoms)
- Esophageal motility disorders
- Hiatal hernia size and impact
Surgery is an option for a small group. Fundoplication-wrapping the top of the stomach around the LES-has a 90% success rate at 10 years. Newer options like the LINX® device (a magnetic bracelet around the LES) or TIF (transoral incisionless fundoplication) offer less invasive alternatives with 85%+ symptom reduction at 5 years.
But surgery isn’t for everyone. It’s usually reserved for people with clear anatomical issues who’ve failed medical therapy.
Final Takeaway: You Have More Control Than You Think
GERD isn’t something you just have to live with. It’s not inevitable. You don’t need to be on PPIs forever. Most people can manage it well with a mix of smart habits and short-term medication. The key is not to treat the symptom alone-you need to fix the pattern.Start today: write down your last 3 meals and when you felt symptoms. Look for patterns. Cut out your biggest trigger. Go to bed 3 hours after eating. Give it 2 weeks. If you feel better, you’re on the right track. If not, talk to your doctor-not just about more pills, but about how to reset your whole approach.
GERD is manageable. But it demands your attention. Not because it’s dangerous-but because it doesn’t have to be part of your life.
Can lifestyle changes alone cure GERD?
Yes, for many people. Losing 5-10% of body weight, avoiding trigger foods, and not eating before bed can eliminate symptoms completely in up to 58% of patients. It’s not a quick fix-it takes 2-4 weeks to see results-but it’s the most sustainable solution. Some people never need medication after making these changes.
Are PPIs safe for long-term use?
PPIs are safe for short-term use, but long-term use (over 1 year) carries risks: increased chance of infections, kidney problems, bone fractures, and vitamin B12 deficiency. Guidelines recommend reevaluating PPI use every 8 weeks. If symptoms are under control, try to reduce or stop them with your doctor’s help.
Why do symptoms get worse when I stop PPIs?
This is called rebound acid hypersecretion. When you stop PPIs suddenly, your stomach overproduces acid to make up for the suppressed levels. Symptoms can be worse than before for several weeks. To avoid this, taper off slowly-switch to an H2 blocker like famotidine for 2-4 weeks, then reduce that dose gradually.
What foods should I avoid with GERD?
The top triggers are coffee, tomatoes, alcohol, chocolate, fatty foods, and spicy foods. These relax the lower esophageal sphincter or increase acid production. Not everyone reacts to all of them-keep a food diary for 2 weeks to find your personal triggers. Cutting out just 1-2 major ones often brings big relief.
When should I see a doctor about GERD?
See a doctor if you have symptoms more than twice a week, if over-the-counter meds don’t help, or if you notice warning signs: trouble swallowing, unexplained weight loss, vomiting blood, or black stools. These could signal complications like esophageal strictures or Barrett’s esophagus, which need endoscopy to diagnose.






Sarah Clifford
December 9, 2025 at 21:44
I’ve been on PPIs for 7 years and honestly? I think they’re just making my acid worse. My doctor won’t listen, but I stopped cold turkey last month and now I’m burning through three packs of Tums a day. Who’s to say it’s not the drugs causing this? I swear, Big Pharma is selling us pain.