Bringing a medication action plan to your doctor’s visit isn’t just a formality-it’s one of the most powerful tools you have to avoid dangerous drug interactions, stop taking medicines you no longer need, and actually follow your treatment plan. If you’re on three or more medications, or if you’ve been hospitalized recently, this isn’t optional. It’s essential. And yet, most people still show up with a shoebox of pill bottles or a vague memory of what they’re taking. That’s how mistakes happen.
What a Medication Action Plan Actually Is
A Medication Action Plan (MAP) is a simple, structured form that turns your medication list into a living document. It’s not just a list of pills. It’s a roadmap. It tells you what each medicine is for, when to take it, what to watch out for, and what to do if something goes wrong. The format is standardized across Medicare Part D programs in the U.S. and by law in Germany since 2016. It’s designed so that even someone with low health literacy can understand it.The core sections you’ll find in every reliable template:
- What we talked about - Notes from your provider on changes, concerns, or goals.
- What I need to do - Clear, specific instructions: "Take metformin 500 mg with breakfast and dinner starting tomorrow."
- What I did and when I did it - A tracker for whether you took your meds, missed doses, or had side effects.
- My follow-up plan - When to return, what symptoms to watch for, and a space to write down questions you forgot to ask.
It must be signed by both you and your provider. That signature isn’t just bureaucracy-it’s accountability. If something goes wrong, this document becomes your record.
Why This Works Better Than a List of Pills
A piece of paper with "Lisinopril 10 mg" written on it doesn’t tell your doctor why you’re taking it. Maybe you were prescribed it for high blood pressure. Maybe your doctor switched you from another drug and forgot to update your list. Maybe you stopped taking it six months ago because it made you cough-but you never told anyone.A MAP fixes that. In a 2016 German study, 87.5% of patients using the standardized template could find critical medication info on the first try. Patients who brought their MAP to pharmacy visits improved medication reconciliation by 76.3% compared to those who didn’t. That’s not a small win. That’s life-saving.
And it’s not just about accuracy. Research from the Agency for Healthcare Research and Quality shows that consistent use of MAPs can reduce adverse drug events by up to 23%. That means fewer hospital stays, fewer ER visits, fewer scary moments in the middle of the night.
How to Prepare Before Your Visit
Don’t wait until you’re sitting in the exam room to figure this out. Start three days before.- Collect every medication - Prescription, over-the-counter, vitamins, herbal supplements. Even the ones you only take "as needed." Put them all on the table.
- Update your MAP - Cross out any meds you stopped taking. Write the date you stopped and why. If you ran out and didn’t refill it, note that too. Don’t guess. If you don’t remember, write "Don’t know"-that’s better than being wrong.
- Write down your questions - Use the "Questions I want to ask" section. Examples: "Why am I still taking this?", "Can I cut this pill in half?", "What happens if I skip a dose?"
- Bring the actual bottles - Not just the list. Seeing the label, dosage, and expiration date helps your provider catch mistakes you didn’t even notice.
A 2021 study found that bringing actual pill bottles improved accuracy by 37.2% compared to relying on memory. That’s almost 4 in 10 errors avoided just by showing up with the real thing.
What Happens During the Visit
Your provider should spend the first 5 to 7 minutes reviewing your MAP. If they don’t, speak up. Say: "I brought my Medication Action Plan. Can we go through it together?"Here’s what should happen:
- They check the "What I did" section - If you marked "missed 3 doses last week," they’ll ask why. Was it cost? Side effects? Forgetting? That’s where real care begins.
- They update the list in real time - If you’re starting a new drug, they write the name, dose, start date, and reason. If you’re stopping one, they write the exact date and reason. "Discontinued" isn’t enough. "Stopped on Jan 10 due to dizziness" is.
- They review high-risk meds - Especially if you’re over 65. Medications like benzodiazepines, anticholinergics, or certain painkillers increase fall risk. Your provider should ask: "Are you feeling steadier on your feet?"
- They clarify ambiguous instructions - If your plan says "take as directed," they’ll rewrite it: "Take 1 tablet by mouth every morning with food. Do not take after 6 PM."
Dr. Sarah Spinler, Editor-in-Chief of Pharmacotherapy, says: "The quality of the action plan documentation directly correlates with outcomes. Specific, time-bound action items produce 2.3 times better adherence than general recommendations."

What to Do After the Visit
The visit doesn’t end when you walk out the door.- Update your copy - If your provider made changes, write them in immediately. Don’t wait. Use a pen, not a pencil.
- Share it - Give a copy to your pharmacist, your family caregiver, or anyone who helps you manage your health. The CDC recommends bringing it to emergency rooms too. In 2021, patients who shared their MAP with multiple providers had 22.8% fewer duplicate therapies.
- Keep it accessible - Laminated, in a wallet, or taped to the fridge. A 2023 Reddit thread from a geriatric pharmacist revealed many elderly patients lose their MAPs. Laminated wallet-sized versions work better.
- Review it weekly - Set a reminder on your phone: "Check MAP every Sunday." Are you still taking what’s written? Are there new symptoms? Update it.
Common Mistakes (And How to Avoid Them)
Even with the best intentions, people mess this up. Here’s what goes wrong-and how to fix it:
- Mistake: Writing "take as directed." Fix: Always write exact dose, timing, and purpose. "Take 10 mg of lisinopril every morning for high blood pressure."
- Mistake: Not writing stop dates. Fix: If you stop a med, write the exact date. The Institute for Safe Medication Practices says 18.7% of reconciliation errors come from missing discontinuation dates.
- Mistake: Only using it once a year. Fix: Treat it like a living document. Update it at every visit-even if nothing changed.
- Mistake: Assuming the doctor knows what’s in your pill bottle. Fix: Bring the bottles. Always.
- Mistake: Not asking questions. Fix: Use the "Questions I want to ask" box. Write down three things you’re unsure about. Even if you forget to ask them, your provider will see them.
Who Benefits the Most?
This isn’t just for seniors. It’s for anyone:- Taking 3+ medications
- Seeing multiple doctors
- Have a chronic condition like diabetes, heart failure, or COPD
- Recently discharged from the hospital
- Have trouble remembering doses or side effects
- Have a caregiver helping manage meds
Medicare Part D requires MAPs for 23.7 million beneficiaries. Germany requires it for 70 million people on three or more drugs. This isn’t niche. It’s mainstream care.
What If Your Provider Doesn’t Use It?
Some clinics still don’t have the system set up. That doesn’t mean you shouldn’t bring it.Bring your MAP anyway. Say: "I’ve been using this to keep track of my meds. Can we use it today to make sure everything’s right?"
Most providers will appreciate it. In fact, Dr. Jerry Fahrni of the National Association of Chain Drug Stores says: "The single most effective intervention in reducing medication-related hospitalizations is the consistent use of a standardized Medication Action Plan during every provider encounter."
If they refuse, ask why. Is it because they don’t have time? Offer to fill out the form yourself and hand it to them. If they still won’t use it, consider finding a provider who does. Your safety matters more than convenience.
Final Thought: This Is Your Safety Net
A Medication Action Plan isn’t about paperwork. It’s about control. It’s about knowing exactly what you’re taking and why. It’s about catching errors before they hurt you.One patient in Ohio, Mary Thompson, brought her MAP to a cardiologist appointment and discovered she was taking two blood pressure meds that shouldn’t be combined. That one visit prevented a hospitalization.
You don’t need to be perfect. You just need to be consistent. Update it. Bring it. Ask questions. Share it. That’s how you take charge of your health.
Do I need a Medication Action Plan if I only take one or two medications?
Even if you’re on just one or two meds, a Medication Action Plan is still helpful. It helps you remember why you’re taking them, when to take them, and what side effects to watch for. If you see multiple doctors or get prescriptions from different pharmacies, having a written plan reduces the chance of dangerous interactions or duplicate prescriptions.
Can I use a digital version of the Medication Action Plan?
Yes, many apps and electronic health records now support digital MAPs. But be cautious. Not all digital versions include the required fields like exact stop dates, side effect tracking, or patient-signed confirmation. If you use a digital version, make sure it has the same structure as the paper template: What we talked about, What I need to do, What I did, and My follow-up plan. Always print a copy to bring to appointments-many providers still prefer paper during visits.
What if I can’t read or understand the plan?
You’re not alone. About 12% of U.S. adults have proficient health literacy. Ask your pharmacist or provider to go over it with you in plain language. Many clinics offer visual versions with icons or color-coded boxes. You can also ask a family member or caregiver to help you fill it out and explain it back to you. The goal isn’t perfect writing-it’s understanding.
How often should I update my Medication Action Plan?
Update it every time you see a healthcare provider-whether it’s your doctor, pharmacist, or specialist. Even if nothing changed, confirm it. Also update it immediately if you start or stop a medication, experience a new side effect, or change your routine. Don’t wait for your annual visit. Treat it like a living document.
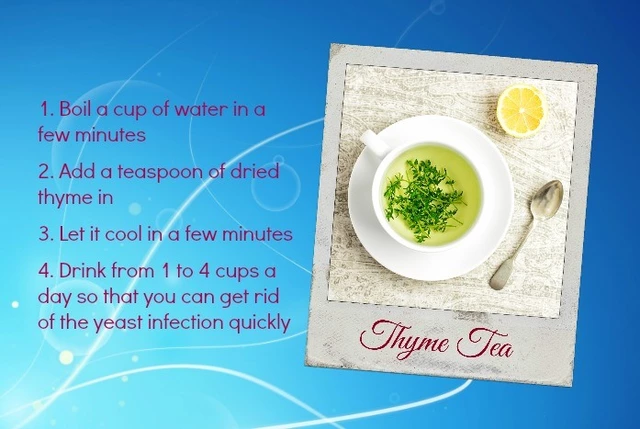
Can my pharmacist help me fill out the Medication Action Plan?
Absolutely. Pharmacists are trained in medication management and are often the best people to help you fill out your MAP accurately. They can check for interactions, clarify dosing, and help you track side effects. Many community pharmacies offer free Medication Therapy Management (MTM) sessions where they’ll review your entire list and update your plan on the spot.
What if I lose my Medication Action Plan?
Call your pharmacist or primary care provider and ask for a copy. Most clinics and pharmacies keep a copy on file. If you’ve been consistent about updating it, they can reconstruct it from your records. In the meantime, write down everything you’re taking from memory and bring it to your next appointment. But don’t wait-get a new copy as soon as possible. Keep a backup at home or with a trusted family member.




Phil Davis
January 27, 2026 at 14:33
I brought my shoebox of pills to my last appointment. The doctor stared at it like it was a cursed artifact. Then she asked if I had a MAP. I said no. She sighed like I’d just admitted I still use dial-up.
Now I have one. It’s laminated. I carry it like a holy relic. My meds don’t scare me anymore. They just sit there, waiting for me to update them.
Also, I stopped taking that fish oil. Didn’t need it. Forgot to tell anyone. Now I won’t.