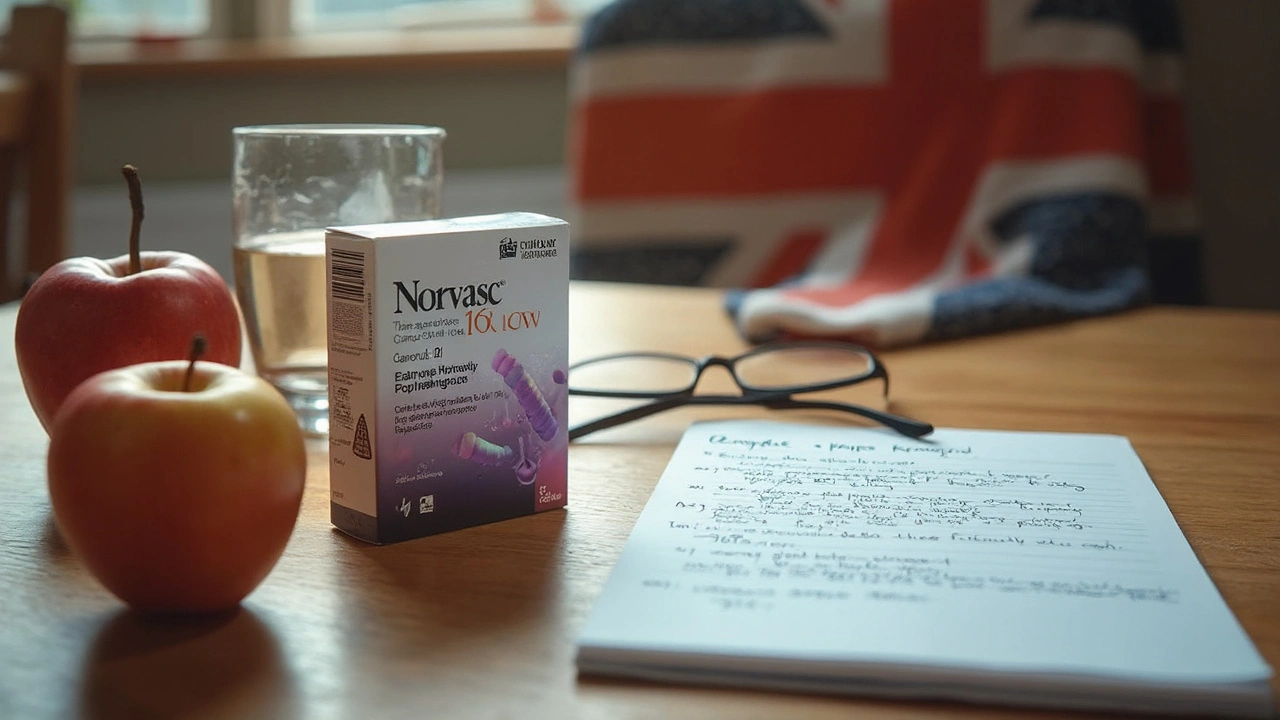
You know what’s more common than mismatched socks? High blood pressure. Doctors hand out Norvasc prescriptions every day, and if you’re reading this, chances are either you or someone close to you is popping those little pills. The thing is, even though Norvasc (generic name: amlodipine) has been around since the ’90s, the details still baffle a lot of people. What does it actually do? Is it as effective as everyone says? Are you suddenly going to start glowing in the dark? (Spoiler: No, you won’t.) But there’s way more to this medication than just lowering your numbers. Let’s pull back the curtain and talk straight about what living with Norvasc really looks like, from the nitty-gritty of daily use to all those little things nobody bothers to mention at the pharmacy.
What Does Norvasc Do, and Who Needs It?
People just call it Norvasc, but pharmacists see it as amlodipine besylate—one of the top prescribed blood pressure drugs worldwide. We’re talking millions of people. Its main job is to relax the blood vessels so blood can move with less resistance. Think of it like traffic control: less squeezing in your arteries means a smoother flow, which in turn drops your blood pressure. Now, Norvasc isn’t some miracle pill that erases all risk; you still have to eat your veggies and move your body. But for anyone battling hypertension or frequent angina (that’s when your heart screams for more oxygen, usually because of narrowed arteries), this tiny tablet makes a huge difference. Studies show Norvasc can also help prevent strokes and heart attacks when part of a doctor-supervised routine.
Here’s an interesting tidbit: Norvasc is what’s called a calcium channel blocker. Basically, it stops calcium from getting into the muscle cells that line your blood vessels and heart. Why does that matter? Because too much calcium tightens things up, like a muscle cramp in your artery. Norvasc tells those cells to chill out, which keeps your vessels wide and pressure steady. That’s not just good for your blood pressure; it’s great for your heart, reducing its workload and risk of damage over time.
A lot of folks first hear about Norvasc at a routine check-up. Maybe your numbers were creeping up, or there were warning signs of heart trouble. Doctors often pick Norvasc because, compared to some other hypertension meds, it’s less likely to upset your electrolytes or cause nagging coughs (looking at you, ACE inhibitors). Plus, for older adults—like my father-in-law, who stubbornly refuses to give up salty foods—Norvasc can be gentler on the kidneys. And while it’s most famous for high blood pressure, Norvasc is also useful for people suffering from Raynaud’s disease, certain types of chest pain, and even sometimes for managing migraines. It’s on the World Health Organization’s list of essential medicines for a reason.
But, don’t just rush out and start treatment. Norvasc is prescription-only for a reason: you need a proper diagnosis, because using it with certain conditions—like very low blood pressure or severe liver disease—can actually cause more harm than good. If you’re pregnant or breastfeeding, doctors weigh the risks carefully, since data on Norvasc in those groups isn’t ironclad. The takeaway? Always talk to your health provider before starting or stopping Norvasc, even if your neighbor swears by it.
Start Smart: Dosage, Side Effects, and What to Expect
Most adults starting Norvasc end up on a 5 mg tablet once per day, but doctors can adjust that depending on your blood pressure goals, age, and other medications. The highest standard dose is 10 mg per day. What’s handy is you don’t need to eat food with it, and you can take it morning or evening—though sticking to the same time every day helps keep things consistent in your system. If you miss a dose, don’t double up; just take it when you remember (unless it’s almost time for the next pill). That sound you hear? It’s the collective sigh of every doctor who’s seen a patient panic and swallow two pills at once. Don’t do that.
Now, what does Norvasc actually feel like? Here’s the honest answer: probably nothing right away. Blood pressure meds like this work quietly. You may not notice anything from your very first pill, which can be a bit anticlimactic. Don’t quit just because you don’t feel ‘better’ instantly. Give it a few weeks—your doctor will likely check your progress around 2-4 weeks in. If your blood pressure or angina isn’t under control, they might raise the dose or add another type of medication.
Side effects—yep, they happen, but not to everyone. The most common one is ankle swelling (edema), showing up in about 1 out of every 10 people. It’s weird but usually harmless. If it bothers you, putting your feet up or wearing compression socks can help. Sometimes the swelling gets bad enough that people switch meds, but for most, it’s more an annoyance than a real danger. You might also get headaches, tiredness, flushing, or dizziness, especially during the first week or so. My wife, Matilda, started Norvasc last year and texted me, “Why do my feet look like loaves of bread?” It faded after a few weeks, and now she barely remembers it ever happened. Nausea and stomach pain are rare, but if you feel them, it’s been reported. Serious side effects like irregular heartbeat or severe allergic reactions are very uncommon, but always call your doctor if you notice anything out of the ordinary.
If you have liver issues or take other heart medicines (especially beta-blockers or other blood pressure drugs), keep your care team in the loop. Norvasc can mix with grapefruit juice in strange ways, raising your risk of side effects, so most doctors say to skip it while you’re on this medication. Also, certain antibiotics, antifungal meds, or even some HIV treatments might change the way Norvasc works in your body—another reason it pays to speak up about every pill, supplement, or herbal tea you use.
Sticking with Norvasc is key, because stopping suddenly can spike your blood pressure and lead to angina attacks. If cost is a worry, know that the generic, amlodipine, is way cheaper and works just as well. Pharmacies now fill nearly all Norvasc scripts with the generic unless doctors specify. If you’re having any trouble affording it, ask about these options; sometimes small details make a big difference for your wallet and your health.

Making Norvasc Work for You: Tips, Myths, and Real-Life Takeaways
There’s a lot of half-baked advice swirling around when it comes to blood pressure meds. Some people swear Norvasc means you never need to change your lifestyle—which couldn’t be further from the truth. Medication is just one part of the game. Healthy eating, regular exercise, stress management, and other habits all play a starring role in keeping your blood pressure steady and your heart ticking strong. Think of Norvasc as your ace in the sleeve, not a free pass to ignore veggies and movement. A real study in 2022 showed that folks who combined their prescribed meds with walking 30 minutes a day needed lower doses and saw fewer side effects over time. Not too shabby, right?
Don’t fall for the ‘natural alternatives’ hype, either. Yes, things like garlic and fish oil can help, but they’re nowhere near as studied—nor as tightly regulated—as Norvasc and other prescription options. Always talk to your provider before mixing supplements with your regime, because some can even boost the risk of side effects or mess with your heart rhythm.
What about alcohol and caffeine? Moderate caffeine (like your morning coffee) is usually fine. Heavy drinking, however, raises blood pressure and can undo Norvasc’s work. If you like an occasional glass of wine, most docs say it’s okay, but no overdoing it. It’s all about balance. I’ll admit that if Matilda and I share a pizza night, we keep the salt to a minimum. Norvasc helps manage the numbers, but why make its job harder?
For folks with memory lapses, using a pill organizer or setting a phone alarm is a lifesaver. Blood pressure doesn’t spike or dip wildly if you keep a steady routine. Travel a lot? Toss your pills in your carry-on so you’re never caught without. And here’s a personal hack: write your next prescription refill date on your calendar the day you start your new pack. Pharmacies can run out, and you don’t want to go even one day without your heart’s backup plan.
Here’s a quick myth-check for anyone nervous about starting Norvasc:
- Norvasc isn’t addictive; it won’t make you dependent. But your heart does get used to having steady help, so stopping suddenly is a bad plan.
- It doesn’t cause weight gain in most people. If you suddenly balloon up, it’s likely fluid retention (swelling) rather than fat—and your doctor can help sort that out.
- If you want to get pregnant, plan ahead and talk to your doctor. There isn’t clear data on Norvasc in pregnancy, so it’s better to have a plan in place first.
For the number nerds out there: A regular blood pressure reading is around 120/80 mmHg, but your doctor might aim for different numbers based on your age and health risks. Don’t chase perfection—chase progress. A drop of just 10 points in your systolic pressure (the top number) reduces your stroke risk by as much as 27%, according to a massive study from the New England Journal of Medicine. That’s huge. Meds like Norvasc can make that difference happen, as long as you stay the course.
Life on Norvasc isn’t about sitting on the sidelines. Plenty of people climb mountains, chase after grandkids, and dance at weddings while taking this medication. If you’re worried or notice anything weird (like sudden chest pain or heartbeat changes), don’t tough it out—reach out to your care team. Most side effects smooth out after the first month, but persistent problems deserve attention. You may need a dose tweak or a switch-up, and that’s totally normal.
Final tip? Write down your questions before every doctor visit. The best control comes from being your own advocate—you’re the expert on your own body, after all. Norvasc is powerful, but it works best when you make it part of a bigger wellness plan. Keep asking, learning, and tuning in to how you feel. You’ve got this.




Alan Kogosowski
July 18, 2025 at 11:15
First of all, this article does a pretty thorough job explaining Norvasc and its typical uses for blood pressure and angina. But it’s worth diving a bit deeper into the pharmacology behind it because understanding exactly how Norvasc (amlodipine) works can empower patients to be more proactive. It’s a calcium channel blocker, meaning it prevents calcium ions from entering the muscle cells of your heart and blood vessels. This causes your vessels to relax and dilate, lowering blood pressure and reducing the heart’s workload.
Now, the dosage really varies depending on individual patient needs, but starting low is key to avoid common side effects like dizziness or swelling, which tend to subside as your body adjusts. One important fact worth mentioning is that Norvasc’s half-life is quite long — roughly 30 to 50 hours — allowing once-daily dosing, which improves adherence.
Also, potential interactions with other medications like beta-blockers or certain statins should be closely monitored by your physician, as these can potentiate side effects or reduce efficacy. Alongside this, it's crucial for patients to maintain lifestyle changes, such as dietary adjustments and exercise, as medication alone won’t fully manage hypertension.
Overall, this piece is a sound primer but could use more emphasis on individualized care plans and patient education to truly optimize outcomes with Norvasc.