Drug shortages aren’t just inconvenient-they’re life-threatening. When a critical antibiotic or insulin runs out, hospitals scramble. Patients delay treatment. Some don’t get help in time. The problem isn’t random. It’s systemic. And it’s been building for years. The solution? Preventive measures-not reactive fixes. Building a resilient pharmaceutical supply chain isn’t optional anymore. It’s a public health necessity.
Why the System Keeps Breaking
Most people don’t realize that 80% of the active ingredients in U.S. drugs come from overseas. China and India produce nearly 70% of them. That’s not a choice-it’s the result of decades of cost-cutting. Companies moved production overseas because labor and regulation were cheaper. But when a port shuts down, a factory has an accident, or a country imposes export restrictions, the ripple effect hits pharmacies and hospitals within weeks. The pandemic showed us how fragile this system is. One factory in India stopped making heparin. Suddenly, hospitals across the U.S. couldn’t perform surgeries safely. Another factory in China shut down during lockdowns. Critical cancer drugs vanished from shelves. These weren’t one-off events. They were predictable failures. The U.S. government now calls this a national security risk. The Department of Defense says it’s not just about medicine-it’s about readiness. If a military base needs antibiotics and they’re stuck in a shipping container halfway across the world, that’s not a logistics problem. It’s a threat to lives.What Resilience Actually Means
Resilience isn’t about making everything in America. That’s unrealistic-and expensive. It’s about having options. The Mathematica Inc. report from 2023 defines it clearly: the ability to anticipate, prepare for, respond to, and recover from disruptions while keeping critical drugs flowing. That means three things:- Preparedness: Knowing where your risks are before they happen.
- Response: Keeping production going even when something breaks.
- Recovery: Getting back to normal fast after a crisis.
Building Buffer Stock-The Simplest Fix
One of the most effective, underused tools? Inventory. Not just any inventory-strategic buffer stock for the medicines that save lives. Right now, most hospitals and pharmacies keep 30 days of inventory for essential drugs. Resilient systems aim for 60 to 90 days. That’s not waste. It’s insurance. The U.S. government is starting to act. In August 2025, an executive order launched the Strategic Active Pharmaceutical Ingredients Reserve. The goal? Store enough raw materials to cover 90 days of demand for 150 critical medicines by 2027. That includes antibiotics, insulin, blood thinners, and anesthetics. This isn’t theoretical. Companies that already use buffer stock saw 23% fewer disruptions during the 2023-2025 crisis period. For a large pharma firm, that meant avoiding $14.7 million in lost revenue per major event-not counting lives saved.Dual-Sourcing: Don’t Put All Your Eggs in One Basket
Relying on one supplier for a critical ingredient is like driving a car with no spare tire. If it fails, you’re stranded. Top-performing companies now dual-source 70-80% of their most important APIs. That means two factories, in two different countries, making the same ingredient. One in India. One in Spain. One in the U.S. One in South Korea. It’s more expensive. But it’s safer. And the cost difference is shrinking. Continuous manufacturing-a newer, more efficient production method-is cutting costs by 20-25% in energy and 15-20% in waste. That helps offset the added expense of having two suppliers. The FDA has approved only 12 continuous manufacturing facilities so far. But that number is rising fast. By 2027, nearly half of all new drug production capacity will use this tech. It’s smaller, faster to build, and more flexible than old batch plants.
Technology Isn’t Optional-It’s the New Backbone
You can’t manage a global supply chain with spreadsheets and phone calls anymore. Leading firms now use AI to predict disruptions 60-90 days in advance. These systems analyze weather patterns, political unrest, shipping delays, factory maintenance schedules, and even social media chatter about raw material shortages. They’re 85-90% accurate. Blockchain is another game-changer. It tracks every batch of medicine from raw material to patient. That cuts counterfeit drugs by 70-75%. In 2024, a pilot program in Europe found that fake cancer drugs dropped from 1 in 100 to 1 in 400 after blockchain was added. And data integration? Huge. Companies that connected their supplier data, inventory systems, and logistics platforms reduced vulnerability detection time from 45 days to just 7.Regional Networks Are Replacing Global Optimization
The old model-produce everything in the cheapest place, ship it everywhere-doesn’t work anymore. The new model? Regional hubs. North America, Europe, Southeast Asia, and Latin America each build their own supply chains for critical drugs. That way, if one region is hit, others can still function. By 2030, McKinsey predicts that 65-70% of U.S. pharmaceutical needs will be met by regional networks, up from 55% today. Domestic production will rise to 35-40%-not because we can make everything here, but because we need to make the most vital things here. The U.S. currently makes only 28% of essential APIs. For sterile injectables? Just 12%. For antibiotics? 17%. That’s not enough. The government is investing $1.2 billion through the CHIPS and Science Act to fix this. An additional $800 million is proposed for 2025.What’s Holding Companies Back?
It’s not lack of knowledge. It’s lack of action. Most companies know what to do. But they don’t do it. Why?- Silos: 78% of companies say their supply chain, finance, and R&D teams don’t talk to each other.
- Data chaos: 65% still use outdated systems that don’t talk to suppliers’ platforms.
- Regulatory fear: 52% are scared to adopt new tech because they don’t know if the FDA will approve it.

The Cost of Doing Nothing
Building resilience costs money. Companies investing 8-10% of their supply chain budget see a 1.8x return in under three years. But the cost of not investing? Far higher. A single drug shortage can cost a hospital $1.2 million in emergency purchases, overtime, and delayed procedures. For patients, it’s worse. Studies show that delays in cancer treatment due to drug shortages reduce survival rates by up to 18%. And it’s not just about drugs. When a hospital can’t get a sedative for an ICU patient, they use a less effective alternative. That increases complications. Longer stays. Higher costs. More deaths.What You Can Do-Even If You’re Not a Pharma Giant
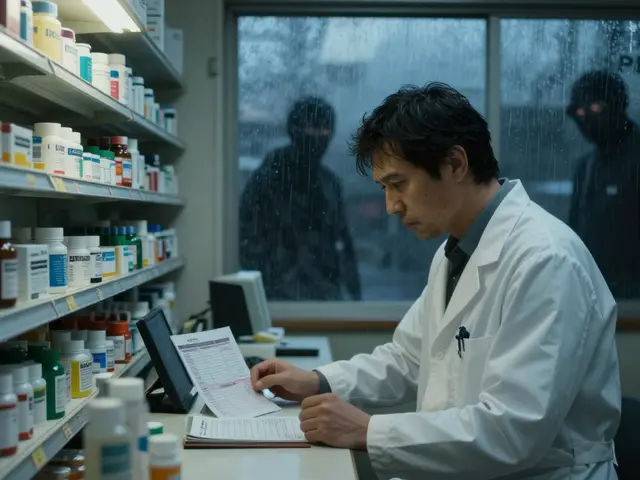
You don’t need to be Pfizer to make a difference. If you’re a pharmacist: Track your top 10 most critical drugs. Ask your distributor: Do they have a second supplier? What’s your backup plan? If you’re a hospital administrator: Push for 60-90 days of buffer stock for life-saving drugs. Make it part of your emergency plan. If you’re a policymaker or investor: Support companies that dual-source. Reward transparency. Fund continuous manufacturing. Don’t just talk about resilience-fund it.The Future Isn’t About Going Back-It’s About Building Forward
We can’t go back to the way things were. Globalization didn’t fail. It just exposed its limits. The future is balanced. A mix of domestic capacity for the most critical drugs. Regional networks for stability. Global partnerships for efficiency. Technology for speed. And inventory as a safety net. The goal isn’t perfection. It’s reliability. When someone needs a drug, it should be there-not because of luck, but because the system was built to work. The tools exist. The data is there. The cost of action is lower than the cost of inaction. The question isn’t whether we can build resilient supply chains. It’s whether we’re willing to.What are the main causes of pharmaceutical supply chain disruptions?
The main causes include geopolitical tensions, natural disasters, factory shutdowns, export bans, labor strikes, and regulatory delays. Over 80% of active pharmaceutical ingredients (APIs) are produced overseas, primarily in China and India, making supply chains vulnerable to regional disruptions. The COVID-19 pandemic exposed how quickly these dependencies can break down.
How does dual-sourcing improve supply chain resilience?
Dual-sourcing means having two or more suppliers for the same critical ingredient, ideally in different geographic regions. This reduces the risk of total supply loss if one supplier fails. Leading companies now dual-source 70-80% of their essential APIs, cutting disruption risk by up to 60%. It’s more expensive upfront, but prevents costly shortages and maintains patient access.
What is continuous manufacturing, and why is it important?
Continuous manufacturing is a modern production method that runs drug production nonstop in a single, integrated system, unlike traditional batch processing. It reduces facility footprint by 30-40%, cuts energy use by 20-25%, and lowers waste by 15-20%. It’s faster to build (12-18 months vs. 3-5 years) and more flexible. The FDA is accelerating approvals for these systems, and by 2027, nearly half of new production capacity will use this tech.
Why isn’t bringing all drug production back to the U.S. the solution?
Bringing everything home isn’t practical or cost-effective. The U.S. lacks the skilled workforce, infrastructure, and scale to produce all APIs domestically. Experts warn that over-reliance on domestic supply creates new risks, like single-point failures. The goal isn’t isolation-it’s balance: produce critical drugs domestically, diversify globally, and use technology to manage risk.
How can small pharmacies or clinics contribute to supply chain resilience?
Small pharmacies can track their top 5-10 critical medications and ask distributors about backup suppliers. They can maintain 60-90 days of inventory for life-saving drugs like insulin, antibiotics, and epinephrine. They can also report shortages to state health departments to help identify systemic issues early. Every small action adds up.
What role does AI play in preventing drug shortages?
AI analyzes global data-weather, politics, shipping delays, factory maintenance, and even social media-to predict disruptions 60-90 days in advance with 85-90% accuracy. It helps companies shift orders, adjust inventory, or activate backup suppliers before a shortage hits. Companies using AI see faster response times and fewer missed deliveries.
What is the Strategic Active Pharmaceutical Ingredients Reserve?
Launched in August 2025 by executive order, this U.S. government initiative aims to stockpile raw materials for 150 essential medicines, ensuring a 90-day supply during emergencies. It targets critical drugs like antibiotics, insulin, and anesthetics. The reserve is designed to prevent shortages before they start, acting as a national safety net.
How long does it take to build a new pharmaceutical manufacturing facility?
Traditional batch manufacturing plants take 3-5 years to build and approve. New modular or container-based facilities can be deployed in 12-18 months. Continuous manufacturing systems, which are smaller and more flexible, also speed up the process. Regulatory approvals are improving too-the FDA now cuts approval timelines from 2-3 years to 12-18 months for qualified continuous manufacturing sites.



Michael Dillon
December 24, 2025 at 09:24
I get the urgency, but let's be real-building buffer stocks is just a Band-Aid. The real problem is that we let corporations optimize for quarterly profits instead of human survival. We're treating medicine like smartphones now. Replace it, upgrade it, toss it when it's inconvenient. This isn't resilience. It's capitalism with a stethoscope.