An adrenal incidentaloma is a lump on the adrenal gland that shows up by accident-usually during a CT or MRI scan done for something else, like back pain or a car accident. It’s not something you feel, and most people don’t know they have one until their doctor points it out. These masses are surprisingly common: about 1 in 50 adults has one, and that number jumps to more than 1 in 14 for people over 70. The big question isn’t whether it’s there, but whether it’s dangerous.
What Makes an Adrenal Mass Risky?
Not all adrenal tumors are the same. In fact, about 8 out of 10 are harmless, non-functioning adenomas that will never cause problems. But the other 2 out of 10? Those are the ones that can kill you if you miss them. There are three main types of adrenal incidentalomas:- Functioning tumors-these make too much hormone. That means they can cause high blood pressure, weight gain, muscle weakness, or even heart rhythm problems.
- Malignant tumors-either primary adrenal cancer (adrenocortical carcinoma) or cancer that spread from elsewhere, like lung or breast cancer.
- Benign non-functioning tumors-these sit quietly and do nothing. Think of them like a mole on your skin-present, but not harmful.
The goal of evaluation isn’t to remove every lump. It’s to find the ones that need action-and leave the rest alone.
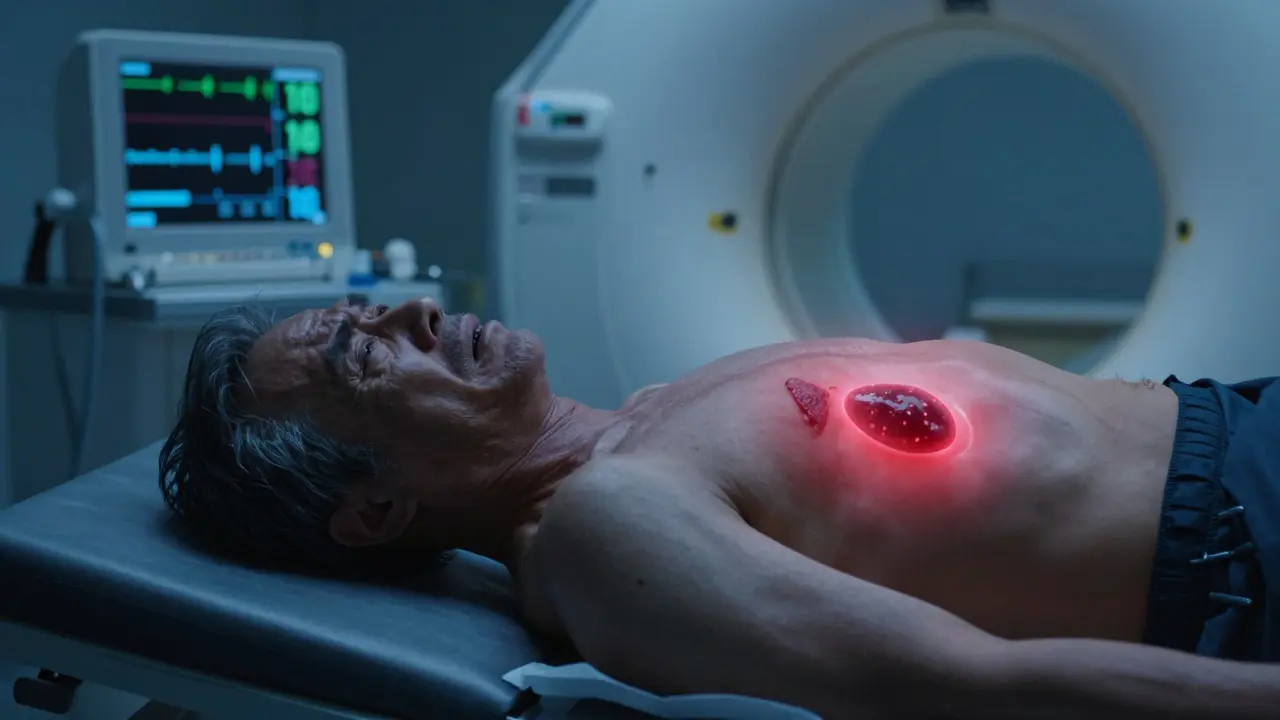
The First Step: Imaging
The first test after finding an adrenal mass is almost always an unenhanced CT scan. Why? Because it’s fast, cheap, and tells you a lot. If the tumor has a density below 10 Hounsfield units, there’s a 70-80% chance it’s a benign adenoma. That’s like getting a green light. No further imaging is needed unless other red flags show up. But if the mass looks irregular, has uneven edges, or is larger than 4 cm, that’s a red flag. Tumors bigger than 6 cm have a 25% chance of being cancer. That’s not a small risk. That’s a reason to act.Testing for Hormones: The Real Deal
Size alone doesn’t tell the whole story. A tiny tumor can be deadly if it’s making too much adrenaline. That’s why every single adrenal incidentaloma needs three key hormone tests:- Pheochromocytoma screen-this is non-negotiable. You test for metanephrines in the blood or urine. If you skip this and operate on a pheochromocytoma, the stress of surgery can trigger a deadly surge in blood pressure. It’s happened before. It shouldn’t happen again.
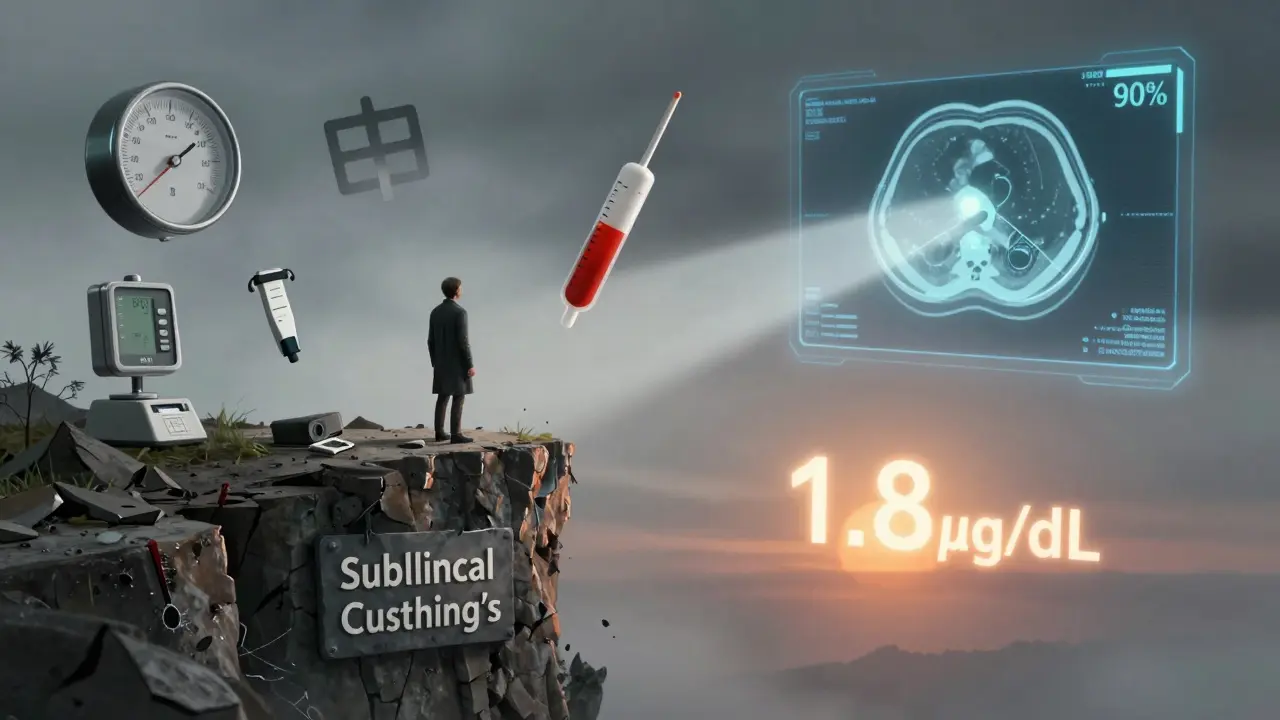
- Cortisol overproduction-you give a 1 mg dose of dexamethasone at night and check cortisol the next morning. If it’s above 1.8 μg/dL, you’ve got subclinical Cushing’s. That’s not full-blown Cushing’s disease, but it’s still dangerous. These patients have higher rates of diabetes, high blood pressure, and heart disease-even if they don’t look sick.
- Aldosterone test-only if the patient has high blood pressure or low potassium. This checks for primary hyperaldosteronism, which causes stubborn hypertension. It’s found in about 4% of incidentalomas.
Here’s the catch: not every hospital can run these tests. Only 45% of community hospitals have immediate access to plasma metanephrine testing. That means patients in rural areas or smaller clinics often wait weeks-or get misdiagnosed.
When Do You Operate?
Surgery isn’t the default. It’s the last step-for the right reasons. You remove the adrenal gland if:- The tumor is bigger than 4 cm
- It’s making hormones (pheochromocytoma, cortisol, aldosterone)
- It looks like cancer on imaging (irregular shape, uneven texture, rapid growth)
- It grows more than 1 cm in a year
For pheochromocytomas, surgery isn’t just about removing the tumor-it’s about preparing for it. Patients need alpha-blockers for at least 7-14 days before surgery. This stabilizes blood pressure and prevents a surgical emergency. Skipping this step is dangerous.
For cortisol-producing tumors, surgery improves metabolic health. Studies show patients see better blood sugar control, lower blood pressure, and less weight gain after removal-even if they didn’t have obvious symptoms before.
But if the tumor is under 4 cm, doesn’t make hormones, and looks like a classic adenoma? No surgery. No follow-up. Just file it away. That’s what the Endocrine Society says. And that’s what most experts agree on.
The Gray Zone: Subclinical Cushing’s
This is where things get messy. About 5-10% of incidentalomas produce just enough cortisol to mess with your metabolism-but not enough to make you look like a textbook Cushing’s patient. No moon face. No purple stretch marks. Just high blood pressure, belly fat, and insulin resistance. For years, doctors debated: Should we operate? Or just watch? New data from 2023 says: operate if the post-dexamethasone cortisol level is above 5.0 μg/dL. Those patients have clear metabolic damage. Surgery reverses it. But if it’s between 1.8 and 5.0? That’s still unclear. Some centers watch. Others operate. It depends on the patient’s age, diabetes risk, and how much they’re willing to tolerate long-term health risks.What About Tiny Tumors? Under 1 cm?
Most guidelines say: if it’s under 1 cm, it’s not an incidentaloma. But Japan’s endocrine society disagrees. They say even small masses can be dangerous if they’re functional. In the U.S., we usually ignore them unless they’re in someone with a history of cancer or other risk factors. But if you’re 65 and have a 0.8 cm mass that’s growing? That’s worth a second look.Who Should You See?
This isn’t a general practitioner’s job. It’s a team sport. You need:- An endocrinologist to order and interpret hormone tests
- A radiologist who’s seen hundreds of adrenal masses
- An adrenal surgeon who does this regularly
Patients treated at specialized adrenal centers report 92% satisfaction. Those treated in general hospitals? Only 68%. Why? Because specialists know what to look for. They know when to push for advanced tests like urinary steroid metabolomics-a new tool that’s 92% accurate at spotting cortisol overproduction.
There are only 37 hospitals in the U.S. designated as Comprehensive Adrenal Centers. If you’ve been told you have an adrenal incidentaloma, ask: Is this being managed by someone who sees this every week?
The Hidden Cost: Anxiety and Misinformation
Behind every adrenal mass is a person scared out of their mind. An informal survey of 142 patients found 78% felt intense anxiety while waiting for test results. Many turned to Reddit forums, YouTube videos, or alternative health sites-where misinformation runs wild. Some think adrenal tumors are caused by stress. Others believe supplements can shrink them. The truth? Adrenal incidentalomas aren’t caused by lifestyle. They’re not caused by stress. They’re just… there. Like gray hair. Most are harmless. But a few aren’t. And that’s why the evaluation matters.What’s Changing in 2026?
The Endocrine Society is updating its guidelines this year. New evidence shows that even mild cortisol excess increases heart disease risk. That means we’ll likely see more people getting surgery for subclinical Cushing’s. New tests are emerging too. Urinary steroid metabolomics is replacing the dexamethasone test in top centers. It’s more accurate, doesn’t require taking a pill, and gives results faster. And AI is starting to help radiologists. Algorithms can now analyze CT scans and predict malignancy with over 90% accuracy-better than most human readers.Bottom Line
You don’t need to panic if you have an adrenal incidentaloma. But you do need to act smart.- Get the right tests: metanephrines, dexamethasone suppression, aldosterone/renin.
- Don’t skip the CT density check-10 HU or less? Likely harmless.
- If it’s over 4 cm, growing fast, or making hormones? See a specialist.
- If it’s small, quiet, and looks benign? You’re probably fine. No surgery. No follow-up.
Most adrenal masses are nothing. But one in five could be serious. Don’t assume. Don’t ignore. Get the right evaluation-and don’t settle for a rushed answer from a clinic that’s never seen this before.



Candice Hartley
January 26, 2026 at 18:55
Wow, this is so much more complicated than I thought. I had a 0.9cm nodule last year and my doctor just said 'watch and wait.' I didn't even know there were hormone tests needed.