When someone is deeply depressed, it’s easy to assume it’s just unipolar depression. But what if it’s not? What if the same symptoms are part of something bigger-something that responds to completely different treatments? Misdiagnosing bipolar depression as unipolar depression doesn’t just delay help-it can make things worse. And it happens more often than you think.
What’s the Real Difference?
Unipolar depression, also called Major Depressive Disorder (MDD), means you experience prolonged periods of low mood, fatigue, loss of interest, and other classic depression symptoms-but no history of mania or hypomania. That’s it. No highs. Just lows. Bipolar depression is different. It’s the low phase of bipolar disorder. People with this condition have had at least one episode of mania (intense energy, impulsivity, reduced need for sleep) or hypomania (a milder, shorter version). Even if they’re in a deep depression right now, their brain has shown it can flip into high gear. That’s the key. The DSM-5, the standard guide used by psychiatrists since 2013, makes this distinction clear. But in real life, people often don’t remember or report past manic episodes. They come in saying, “I’ve been down for months.” And if the doctor doesn’t ask the right questions, they’ll get labeled with unipolar depression-wrongly.How Do the Symptoms Differ?
On the surface, both conditions look the same: sadness, trouble sleeping, no motivation. But subtle differences exist-and they matter. People with bipolar depression are more likely to:- Wake up hours before sunrise, unable to go back to sleep
- Feel their mood is worst in the morning and improves slightly by evening
- Experience extreme mental slowing-like their thoughts are stuck in mud
- Have trouble concentrating so badly it affects work or decision-making
- Develop psychotic symptoms, like hearing voices or believing false things during their low phase
Why Misdiagnosis Is So Common-and Dangerous
About 40% of people with bipolar disorder are first diagnosed with unipolar depression. Why? Because they don’t mention mania. They might not recognize it as abnormal. “I just had a really good week,” they say. Or they feel guilty about it. Or they forget. Worse, doctors don’t always ask. A 2018 study found that nearly 37% of cases were misdiagnosed at first. And the consequences? They’re serious. If someone with bipolar depression is given an antidepressant alone-say, sertraline or escitalopram-they’re at high risk of triggering a manic episode. In fact, the STEP-BD study showed that 76% of bipolar patients on antidepressants without mood stabilizers had their mood destabilize. That means they went from depressed to manic, or started cycling rapidly between moods. One Reddit user, u/BipolarSurvivor, shared: “I was on Prozac for 7 years. I went from 2 episodes a year to 12. My psychiatrist didn’t notice the hypomania until I was hospitalized after a spending spree.” That’s not rare. In a 2017 study, people misdiagnosed with unipolar depression spent an average of 8.2 years on the wrong treatment. Over 60% ended up hospitalized because of antidepressant-induced mania.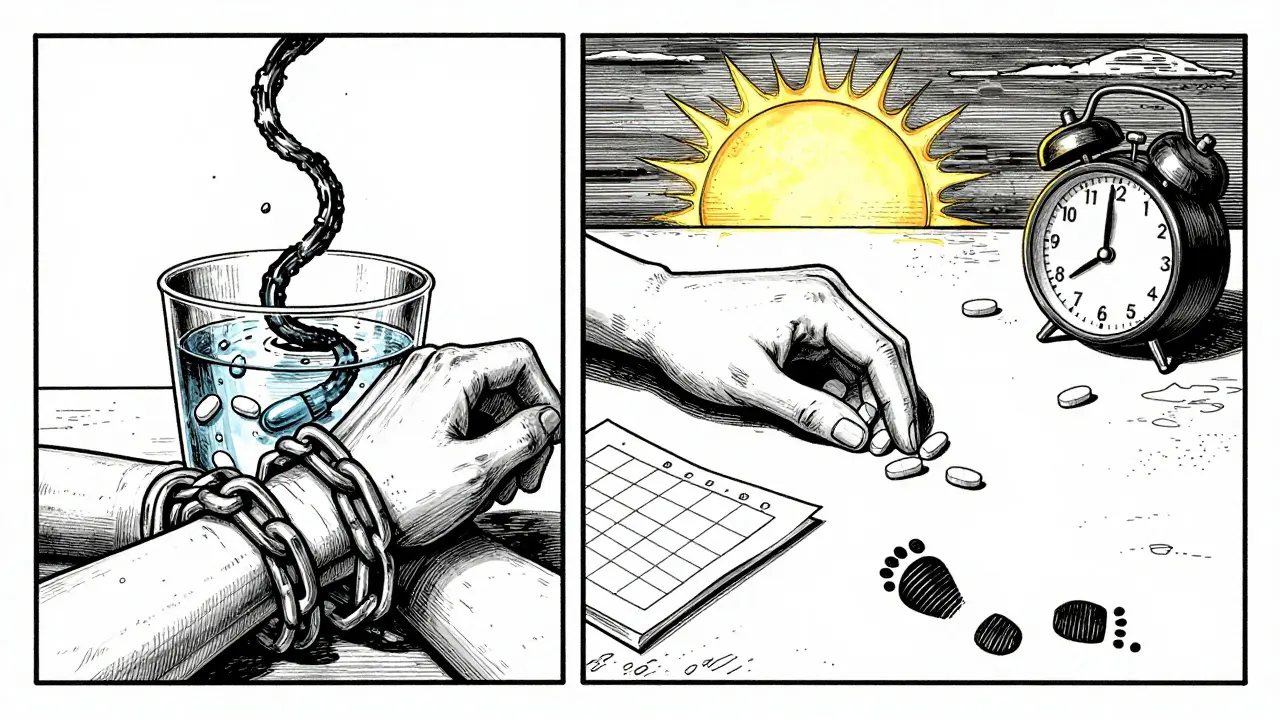
Treatment: One Size Does NOT Fit All
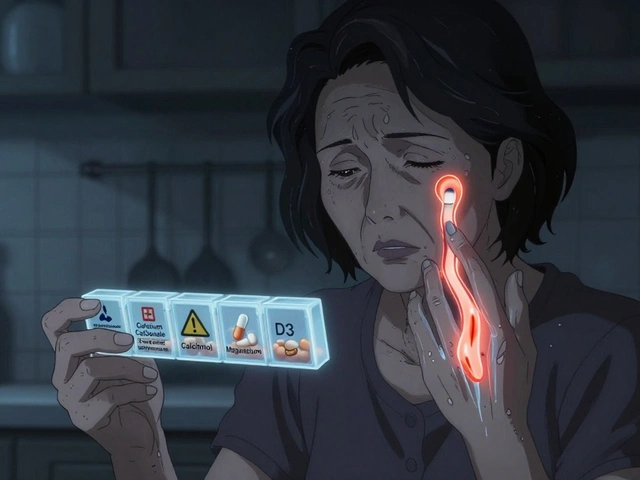
This is where the biggest difference lies. For unipolar depression, first-line treatment is usually an SSRI-medications like sertraline, escitalopram, or fluoxetine. About 60-65% of people respond within 8-12 weeks. If that doesn’t work, doctors may switch to an SNRI like venlafaxine. Therapy like CBT is also highly effective. For bipolar depression? Antidepressants alone are risky. First-line treatment is mood stabilizers or atypical antipsychotics.- Lithium has been used for decades. It reduces depressive episodes by nearly half compared to placebo.
- Quetiapine (Seroquel) is FDA-approved for bipolar depression. In trials, 58% of people improved versus 36% on placebo.
- Lurasidone (Latuda) and cariprazine (Vraylar) are newer options with strong evidence for reducing depressive symptoms without triggering mania.
Screening Tools: What Doctors Should Ask
You can’t rely on a patient’s memory. That’s why screening tools exist. The Mood Disorders Questionnaire (MDQ) asks 13 yes/no questions about manic symptoms. A score of 7 or more suggests bipolar disorder. It’s not perfect-it misses a lot-but it’s specific. If someone scores high, further testing is needed. The Hypomania Checklist-32 (HCL-32) is more sensitive. It catches subtler signs of hypomania, like increased talkativeness, risky behavior, or feeling unusually confident. A score above 14 raises serious concern. Doctors should also ask:- “Have you ever felt so good or so irritable that your behavior got you in trouble?”
- “Did your depression get worse after starting an antidepressant?”
- “Do you have a family member with bipolar disorder or who’s been hospitalized for mood swings?”
- “Have you ever had a period where you needed very little sleep but felt full of energy?”
What About Treatment Resistance?
If someone has tried two or more antidepressants and still feels depressed, that’s a warning sign. The STAR*D study found these patients are 3.7 times more likely to have bipolar disorder than those who responded to medication. That doesn’t mean they should be switched to lithium right away. But it does mean the diagnosis needs re-evaluation. And if someone has mixed features-depression with some manic symptoms like racing thoughts or irritability-DSM-5-TR (2022) allows doctors to add a “with mixed features” label. That’s a step toward recognizing the spectrum, even if the full diagnosis isn’t clear yet.
Long-Term Outlook: Lifelong Management vs. Time-Limited Care
Unipolar depression often responds well to short-term treatment. After one episode, if someone stays well for 6-12 months, many doctors will slowly taper off medication. Relapse risk? About 37% if stopped, 22% if continued. Bipolar disorder is different. It’s usually lifelong. Stopping mood stabilizers leads to relapse in 73% of people within five years. That’s why most people with bipolar disorder stay on medication indefinitely. It’s not about being “cured.” It’s about managing a chronic condition. Regular sleep, avoiding alcohol, stress management, and therapy are just as important as pills.What’s New in Treatment?
The field is evolving. In 2019, the FDA approved esketamine (Spravato) nasal spray for treatment-resistant unipolar depression. It works fast-some feel better in hours. But it’s expensive, requires clinic visits, and isn’t approved for bipolar depression yet. For bipolar depression, cariprazine showed 36.6% remission rates in trials-better than placebo. It’s now a standard option. And research is moving beyond symptoms. A 2023 Lancet study found a 12-gene pattern that can distinguish bipolar from unipolar depression with 83% accuracy. That’s not in clinics yet, but it’s coming. Smartphone apps that track sleep, voice tone, typing speed, and location are also being tested to detect early mood shifts before they become full episodes.Final Takeaway: Diagnosis Changes Everything
Bipolar depression and unipolar depression aren’t just two versions of the same thing. They’re different illnesses with different causes, different treatments, and different outcomes. Getting the diagnosis right isn’t academic. It’s life-changing. One wrong medication can send someone into a cycle of hospitalizations. The right one can bring stability, work, relationships, and peace. If you’ve been diagnosed with depression and:- Antidepressants didn’t help-or made things worse
- You’ve had periods of high energy, impulsivity, or irritability
- Family members have bipolar disorder or have been hospitalized for mood swings
- You’ve had rapid mood shifts or cycling (4+ episodes a year)
Can you have bipolar depression without ever having mania?
No. By definition, bipolar depression is part of bipolar disorder, which requires at least one past episode of mania or hypomania. If someone has only ever had depressive episodes, they have unipolar depression. However, some people don’t remember or recognize past hypomanic episodes-they might have thought they were just being productive or “on top of the world.” That’s why doctors ask detailed questions about energy levels, sleep needs, and risky behavior.
Are antidepressants always bad for bipolar depression?
Not always, but they’re dangerous alone. Antidepressants can trigger mania, rapid cycling, or worsen mood swings in bipolar disorder. That’s why guidelines say they should never be used as the only treatment. If used at all, they’re added only after a mood stabilizer like lithium or quetiapine is already in place-and even then, they’re often avoided because their benefit is small and risks remain.
How do I know if my depression is treatment-resistant?
If you’ve tried two or more different antidepressants at full doses for at least 6-8 weeks each and still feel severely depressed, you may have treatment-resistant depression. That’s a red flag for possible bipolar disorder. Studies show people with this pattern are over three times more likely to have bipolar depression than unipolar. Don’t just try another pill-ask for a full mood disorder evaluation.
Can bipolar depression turn into unipolar depression?
No. Once someone has had a manic or hypomanic episode, they have bipolar disorder. Even if they haven’t had a high episode in years, the diagnosis doesn’t change. But some people go long periods without mania-sometimes decades. That doesn’t mean they’re cured. It means their illness is stable, usually because they’re on the right treatment.
Is bipolar depression more serious than unipolar depression?
Both are serious. But bipolar depression carries additional risks: higher rates of suicide attempts, more frequent hospitalizations, and the danger of antidepressant-induced mania. People with bipolar disorder also tend to have more comorbid conditions like anxiety, substance use, or metabolic issues. The complexity makes it harder to treat, not necessarily worse-but the stakes are higher if mismanaged.





Allie Lehto
January 24, 2026 at 14:06
i just read this and cried. like... seriously. i was on lexapro for 5 years and no one ever asked about the time i stayed up for 72 hours painting my whole apartment neon pink and bought 3 motorcycles. i thought i was just "having a good phase." turns out i was hypomanic. now i’m on lithium and actually sleeping. thank you for writing this.