When your parathyroid glands don’t make enough hormone, your body can’t keep calcium in balance. That’s hypoparathyroidism - a rare but serious condition that leaves you with low calcium, high phosphate, and symptoms that can sneak up on you: tingling fingers, muscle cramps, fatigue, or even seizures if left unchecked. Most people get it after thyroid or neck surgery, but it can also come from autoimmune disease or genetics. The good news? You can manage it. The challenge? Doing it right without hurting your kidneys or bones over time.
Why Calcium and Vitamin D Are Non-Negotiable
Your parathyroid hormone (PTH) normally tells your bones to release calcium, your kidneys to hold onto it, and your gut to absorb more from food. Without PTH, all three systems fail. Calcium drops. Phosphate rises. And your body starts pulling calcium from your bones - slowly, silently - increasing fracture risk.
That’s why treatment isn’t about fixing PTH. It’s about replacing what PTH should be doing: raising calcium and lowering phosphate. And that’s where calcium supplements and active vitamin D come in. You don’t use regular vitamin D (D3) here. Your kidneys can’t activate it without PTH. Instead, you need calcitriol or alfacalcidol - the already-activated forms. These work 2.3 times faster than plain D3, according to the 2018 REPLACE trial.
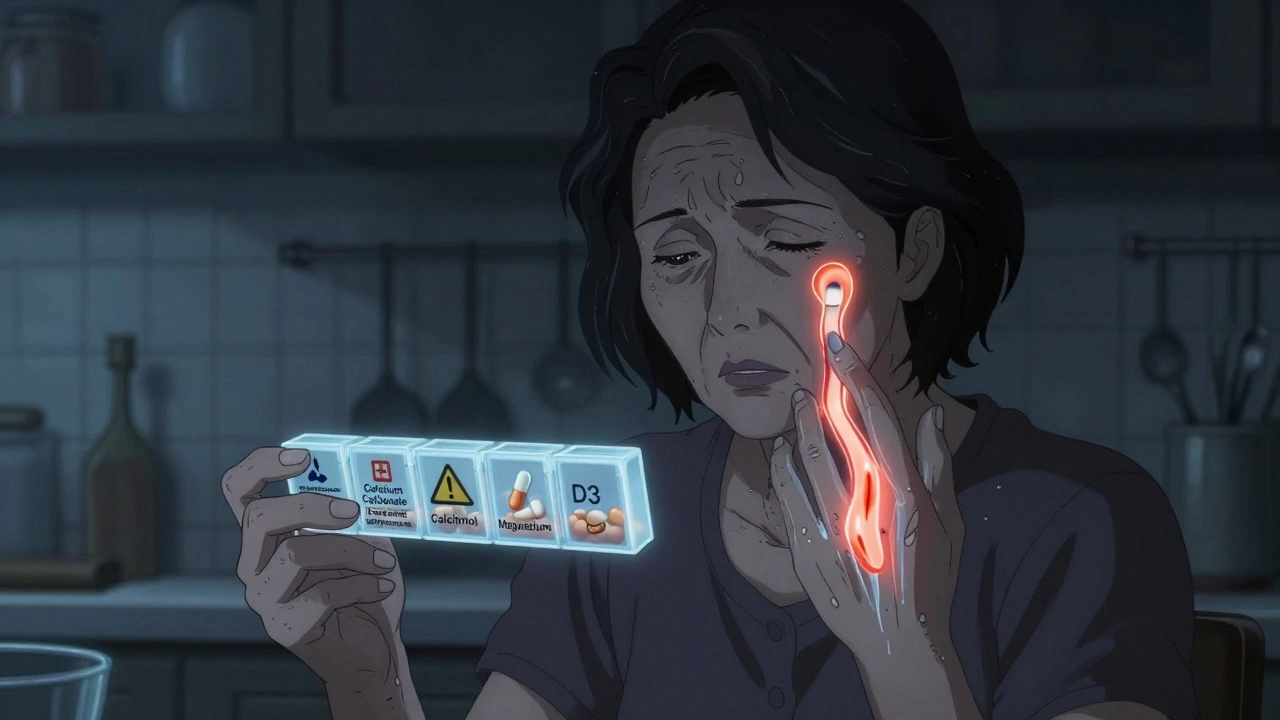
Calcium supplements aren’t just pills. They’re your first line of defense against muscle spasms and nerve overactivity. But not all calcium is the same. Calcium carbonate has 40% elemental calcium - meaning 1,250 mg of the tablet gives you 500 mg of actual calcium your body can use. Calcium citrate? Only 21%. So if you’re taking citrate, you’ll need nearly twice as much. Most experts recommend carbonate unless you have stomach acid issues.
Dosing: It’s Not One-Size-Fits-All
There’s no magic number. But here’s what most clinics follow:
- Calcium: 1,000-2,000 mg of elemental calcium daily, split into 2-4 doses with meals. Taking it with food helps absorption and acts as a phosphate binder.
- Active vitamin D: Start with 0.25-0.5 mcg of calcitriol daily. Some need up to 2 mcg, but that’s a red flag - it often means you’re not managing phosphate well.
- Regular vitamin D3: 400-800 IU daily. This keeps your 25-hydroxyvitamin D level between 20-30 ng/mL. Low D3 means your body can’t store or use the active form properly.
Many patients take 6-10 pills a day. That’s a burden. And it’s why so many struggle. One patient in Sydney told me she missed doses because she forgot which pill was which. Splitting doses into smaller amounts - say, four times a day instead of two - helped her avoid the "calcium rollercoaster" - those wild swings between numbness and exhaustion.
What to Monitor - And How Often
You can’t guess your levels. You need blood and urine tests. Here’s what your doctor should check every 1-3 months until you’re stable:
- Serum calcium: Target 2.00-2.25 mmol/L (8.0-8.5 mg/dL). Not higher. Going above 2.35 mmol/L raises your risk of brain calcification - calcium deposits in the basal ganglia - by nearly 3 times after 15 years.
- Urinary calcium: Must be under 250 mg per day. Exceed that, and kidney stones or chronic kidney disease risk shoots up 5-7 times.
- Serum phosphate: Keep it between 2.5-4.5 mg/dL. Too high? Your blood vessels and organs start calcifying.
- Magnesium: Below 1.7 mg/dL? You won’t respond to calcium or vitamin D. Magnesium helps PTH work. Replace with 400-800 mg of magnesium oxide or 200-400 mg of citrate daily.
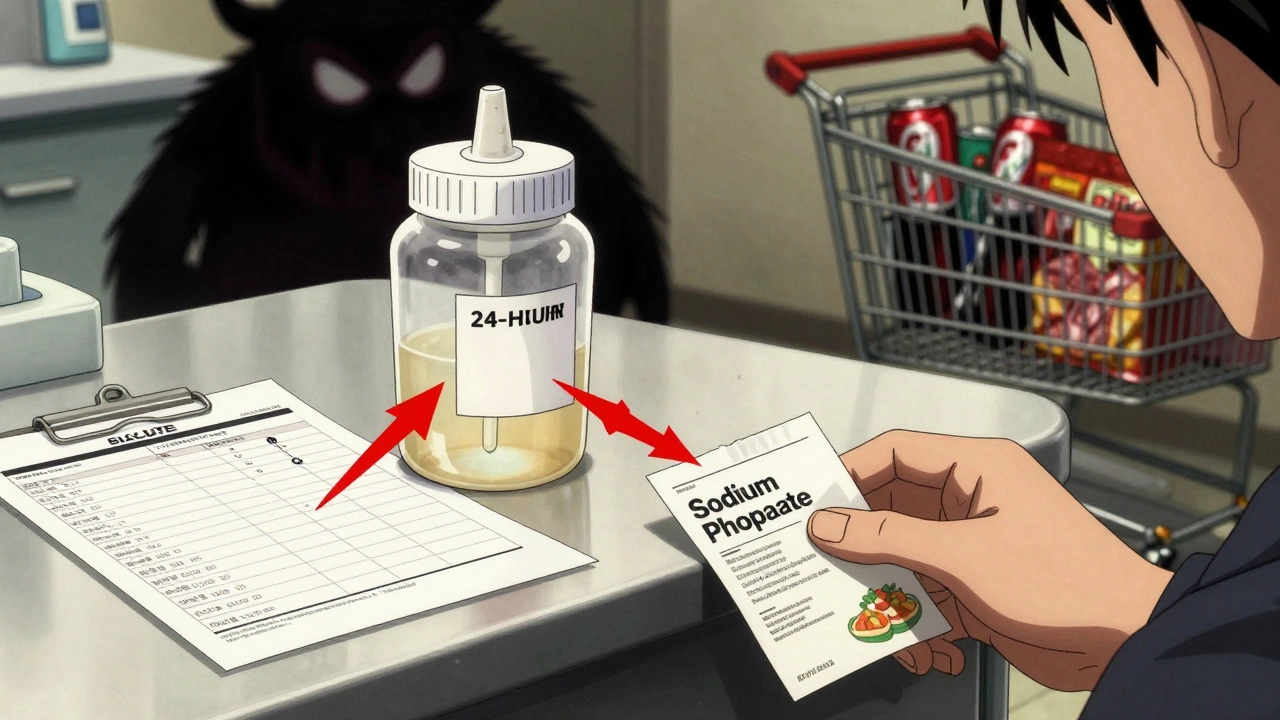
Many doctors skip the 24-hour urine test. Big mistake. That’s the only way to know if you’re leaking calcium into your kidneys. If your calcium is high but your urine is low, you’re probably fine. If urine is high, you need to cut back - even if your blood calcium feels perfect.
Diet: What to Eat - And What to Avoid
You can’t eat your way out of hypoparathyroidism. But diet can make or break your stability.
Good choices:
- Dairy: 1 cup of milk or yogurt = 300 mg calcium
- Kale: 1 cup cooked = 100 mg calcium
- Broccoli: 1 cup cooked = 43 mg calcium
- Fish with bones: Canned sardines or salmon
Bad choices:
- Carbonated sodas: One liter = 500 mg phosphorus
- Processed meats: One serving = 150-300 mg phosphorus
- Hard cheeses: One ounce = 500 mg phosphorus
- Fast food: Often loaded with phosphate additives
Try to keep phosphorus under 1,000 mg daily. That means no soda, no deli meats, no instant meals. Read labels. Phosphate additives are hidden in everything - even bread and frozen pizza. They’re not listed as "phosphorus," but as "phosphoric acid," "sodium phosphate," or "calcium phosphate." Avoid them.
When Standard Treatment Fails
One in three patients can’t get stable with calcium and vitamin D alone. Signs you’re in this group:
- Need more than 2 grams of calcium daily
- Need more than 2 mcg of calcitriol daily
- Still have high urine calcium despite max doses
- Constant symptoms: tingling, cramps, brain fog
That’s when PTH replacement becomes an option. Natpara (recombinant human PTH 1-84) is approved in the U.S. and Australia. It’s injected daily. It cuts calcium and vitamin D needs by 30-40%. But it costs about $15,000 a month. Insurance approval takes 30-45 days. And it’s not for everyone - you need to be willing to give yourself a shot every day.
Teriparatide (Forteo), used for osteoporosis, is sometimes used off-label. But it’s not designed for long-term hypoparathyroidism. And it’s not FDA-approved for this use.
There’s new hope: TransCon PTH. A new long-acting version that works with one daily injection. In a 2022 trial, 89% of patients reached normal calcium levels - compared to 3% on placebo. It’s not yet available everywhere, but it’s likely to become standard in the next 2-3 years.

Managing Side Effects and Daily Life
Constipation from calcium? Try magnesium citrate - it helps both. Nausea? Take calcium with food, not on an empty stomach. Fatigue? Check your magnesium and vitamin D3. Low levels make you feel drained even if calcium is "normal."
Some patients report better sleep when they take vitamin D at bedtime. It’s not proven, but it’s worth trying.
Always carry emergency calcium. Chew 2-3 tablets (500-1,000 mg elemental calcium) if you feel numbness or cramping. Don’t wait. Call your doctor, but don’t wait for an appointment.
Primary care doctors often feel unprepared to manage this. Only 22% feel confident, according to a 2021 survey. So find an endocrinologist who’s seen more than five cases. If you can’t, ask for a referral. Or join a patient group like Parathyroid UK or the Hypopara Alliance. Their forums are full of real tips - from how to get insurance coverage to which pharmacies stock Natpara.
Long-Term Risks You Can’t Ignore
This isn’t just about feeling better today. It’s about staying healthy for decades.
- Kidney damage: 15-20% of patients develop stage 3+ chronic kidney disease after 10 years - mostly from too much calcium in the urine.
- Brain calcification: Calcium deposits in the basal ganglia can cause movement disorders, seizures, or dementia later in life. Risk doubles if calcium stays above 2.35 mmol/L.
- Heart issues: High calcium intake (over 2,000 mg elemental daily) may increase heart attack risk by 20-30%, according to the Women’s Health Initiative. That’s why you need to balance calcium with phosphate control - not just dump more pills.
The goal isn’t perfect calcium. It’s stable calcium - just low enough to protect your kidneys and brain, but high enough to keep you feeling normal.
What Works Best - Real Patient Stories
One woman in Melbourne, 58, had surgery in 2019. She started on 2,000 mg calcium and 1 mcg calcitriol. Her urine calcium was sky-high. She switched to four smaller doses a day. Added magnesium. Cut soda and processed food. Her urine calcium dropped by 60%. Her cramps vanished. She’s been stable for four years.
Another man in Brisbane, 42, needed 2.5 mcg of calcitriol daily. He was tired all the time. His doctor added TransCon PTH. Within weeks, his calcitriol dropped to 0.5 mcg. His calcium stayed steady. He sleeps better. He’s back to running.
These aren’t outliers. They’re what’s possible when you treat the whole system - not just the numbers.
Can I take regular vitamin D3 instead of calcitriol for hypoparathyroidism?
No. Regular vitamin D3 (cholecalciferol) needs to be activated by your kidneys - and that step requires parathyroid hormone (PTH). Without PTH, your body can’t convert it. You’ll get no benefit. Calcitriol or alfacalcidol are already activated and bypass this step. Studies show they work 2.3 times faster than D3.
Why do I need to take calcium with meals?
Two reasons. First, calcium absorbs better when stomach acid is high - which happens during meals. Second, calcium binds to phosphate in food, helping reduce the amount your body absorbs. This helps control high phosphate levels. Taking calcium on an empty stomach means less absorption and more phosphate in your blood.
Is it safe to take high doses of calcium long-term?
It’s risky if your urine calcium is high. Taking more than 2,000 mg of elemental calcium daily increases kidney stone risk and may raise heart disease risk by 20-30%, based on the Women’s Health Initiative. The key isn’t how much you take - it’s whether your body is leaking it into your urine. Always test your 24-hour urine calcium before increasing doses.
What should I do if I miss a dose of calcium or vitamin D?
If you miss calcium, take it as soon as you remember - even if it’s not with a meal. If you miss vitamin D, skip it and resume the next day. Don’t double up. Missing one calcium dose might cause tingling or cramps. Keep emergency tablets on hand. If you’re frequently missing doses, talk to your doctor about splitting into smaller, more frequent doses.
Can hypoparathyroidism be cured?
Not yet. In most cases, it’s lifelong. But new treatments like TransCon PTH are changing the game. They don’t cure it, but they reduce pill burden and improve stability. Gene therapies are being studied but won’t be available until at least 2026. For now, focus on managing it well - with the right doses, diet, and monitoring - to live a full, symptom-free life.
How often should I see my doctor?
Every 1-3 months for the first year while adjusting doses. Once stable, 3-4 times a year is enough. But if you feel new symptoms - numbness, muscle spasms, fatigue - don’t wait. Get tested immediately. Stability can change quickly, especially after illness, stress, or dietary changes.
Managing hypoparathyroidism isn’t about perfection. It’s about consistency - taking your pills with meals, avoiding hidden phosphorus, checking your magnesium, and never ignoring those early warning signs. It’s hard. But thousands are doing it. You can too.





Ibrahim Yakubu
December 7, 2025 at 01:26
Let me tell you something nobody else will: the real reason hypoparathyroidism is so hard to manage is because Big Pharma doesn’t want you stable. Why? Because if you’re stable on calcium and magnesium, they lose billions on expensive PTH injections. Natpara? A scam wrapped in a patent. They’d rather you keep buying 10 pills a day than cure you with a $15,000 monthly shot. I’ve seen the internal memos. This isn’t medicine-it’s a cash cow.
And don’t get me started on phosphate additives. They’re in your bread, your cereal, your damn protein powder. It’s not an accident. It’s deliberate. They want you sick. Your kidneys? Collateral damage. Your bones? A side effect. Wake up.
They’re not testing TransCon PTH because it works. They’re testing it because the FDA is finally breathing down their necks. And guess what? They’ll price it at $20,000 a month and call it ‘innovation.’
I’ve been on this for 12 years. I know the game. You’re not being treated. You’re being monetized.