Probiotic & Antibiotic Compatibility Checker
Check Your Compatibility
This tool helps determine if probiotics are appropriate for your antibiotic treatment based on clinical evidence.
When you're on antibiotics, you know the drill: take your pills, feel better in a few days, and then… the diarrhea hits. Or the bloating. Or the cramps. It’s not just annoying-it can make you feel worse than the original infection. But what if you could stop that before it starts? That’s where probiotics with antibiotics come in. They’re not magic, but for many people, they’re the difference between a rough week and a manageable one.
Why Antibiotics Mess With Your Gut
Antibiotics don’t just kill the bad bacteria causing your infection. They wipe out the good ones too-the trillions of microbes living in your gut that help digest food, make vitamins, and keep your immune system in check. This imbalance is called dysbiosis. And when it happens, harmful bugs like Clostridioides difficile (C. diff) can take over. That’s when things get serious: severe diarrhea, fever, even hospitalization. The good news? You don’t have to just wait it out. Research shows that taking probiotics while on antibiotics can cut your risk of antibiotic-associated diarrhea (AAD) by 42% to 66%. That’s not a small win. It’s the difference between staying home and having to cancel plans-or worse, ending up in the ER.Which Probiotics Actually Work?
Not all probiotics are created equal. If you’re just grabbing the cheapest bottle off the shelf, you might be wasting your money. The science is clear: only certain strains have proven benefits when taken with antibiotics. The two most effective strains, backed by dozens of clinical trials, are:- Lactobacillus rhamnosus GG (often sold as Culturelle)
- Saccharomyces boulardii CNCM I-745 (sold as Florastor)
How to Take Them-Timing Matters
Taking probiotics at the same time as your antibiotic won’t help. The antibiotic will kill the probiotic bacteria before they even get to your gut. So timing is everything. The best practice? Take your probiotic 2 hours after your antibiotic dose. This gives the antibiotic time to do its job without wiping out the good guys. Some people take it in the morning with breakfast and the antibiotic at night, or vice versa. The key is separation. Don’t expect instant results. It takes at least 48 hours for the probiotics to start colonizing and protecting your gut. So start them on day one of your antibiotic course-not when you start feeling sick. And keep taking them. Don’t stop when the antibiotics run out. Continue for at least 1 to 2 weeks after your last dose. That’s when your gut really needs support to rebuild its balance.What About the Risks?
For most healthy people, probiotics are safe. Side effects are rare and mild-maybe a little gas or bloating for the first few days. That usually goes away on its own. But there are exceptions. If you’re immunocompromised-say, you’re on chemotherapy, have an organ transplant, or have a central line catheter-you’re at risk for serious infections from probiotics. There are documented cases of people developing bloodstream infections (bacteremia) from probiotic strains. The FDA and CDC warn against using them in these cases. Also, avoid probiotics if you have severe pancreatitis. Studies show they can make it worse. And here’s a twist: a 2018 study in Cell found that some people who took multi-strain probiotics after antibiotics actually had slower gut recovery than those who didn’t take any. It’s controversial, and not replicated in larger trials, but it’s a reminder: probiotics aren’t one-size-fits-all. If you’re not feeling better-or worse-after a few days, talk to your doctor.
Quality Is a Big Problem
Here’s the ugly truth: many probiotic products don’t contain what’s on the label. Independent testing by ConsumerLab found that 23% to 45% of supplements had inaccurate CFU counts-or sometimes, no live bacteria at all. How do you know you’re getting a good one? Look for these signs:- Refrigerated storage (most live cultures need cold to survive)
- Third-party verification (USP Verified or NSF Certified)
- Clear strain names on the label (not just “probiotic blend”)
- Expiry date and CFU count (should be at least 10 billion per dose)
What About Fecal Transplants?
You might have heard about fecal microbiota transplantation (FMT)-basically, transplanting healthy gut bacteria from a donor. It’s incredibly effective for recurrent C. diff infections, with success rates over 90%. But it’s invasive, expensive, and only used in serious cases. Probiotics aren’t as powerful as FMT for severe infections. But they’re safer, cheaper, and available without a prescription. For preventing diarrhea in most people on antibiotics, probiotics are the practical first step.What Do Doctors Really Think?
There’s no universal agreement. The Infectious Diseases Society of America (IDSA) says it’s okay to use specific probiotics for high-risk patients. The American Gastroenterological Association (AGA) says no-because product quality is so inconsistent. But here’s what most frontline doctors say in private: “If a patient asks, I’ll recommend it.” A 2022 survey found that 62% of U.S. primary care doctors suggest probiotics for patients on antibiotics. Only 28% do it routinely, mostly because they don’t know which brand to trust. The bottom line? If you’re taking antibiotics and worried about side effects, probiotics are worth trying-if you pick the right ones.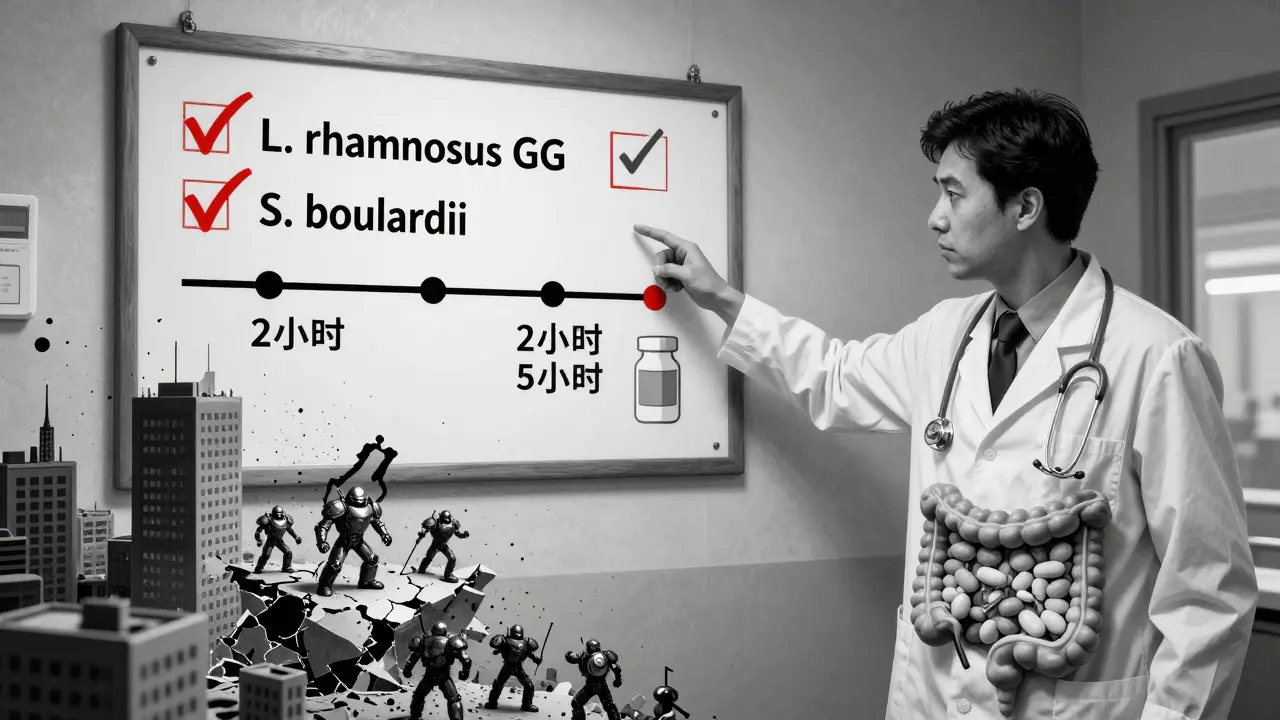
Real People, Real Results
On Reddit, users report the same pattern: > “Took Culturelle with amoxicillin. No diarrhea this time. Finally.” - u/MomOfThree, r/GutHealth > “Spent $35 on Garden of Life. Still got C. diff after clindamycin.” - u/AntibioticSurvivor The difference? One picked a proven strain. The other didn’t. Amazon reviews for Culturelle and Florastor average 4.1 stars out of 5. The most common praise: “No more bathroom emergencies.” The most common complaint: “Didn’t work.” But when you dig into the negative reviews, most of those people used generic brands or didn’t take them at the right time.What’s Next?
Science is moving fast. Researchers are now developing “precision probiotics”-specific blends designed to counteract the damage caused by particular antibiotics. One 8-strain formula called VE303 reduced C. diff by 76% in early trials. But there’s a new concern: a 2025 study found that 38% of commercial probiotics carry antibiotic resistance genes. That means the “good” bacteria might be hiding genes that help bad bacteria fight off antibiotics. The FDA is now requiring new products to be screened for this. For now, stick with the proven strains. Don’t chase the latest hype. Your gut doesn’t need novelty-it needs reliability.Quick Checklist: Probiotics + Antibiotics
- ✅ Start on day one of antibiotics
- ✅ Take probiotic 2 hours after antibiotic
- ✅ Use only L. rhamnosus GG or S. boulardii
- ✅ Choose refrigerated, USP/NSF-certified brands
- ✅ Continue for 1-2 weeks after antibiotics end
- ❌ Don’t use if immunocompromised, on a central line, or with severe pancreatitis
- ❌ Don’t trust unlabeled or unverified products
Antibiotics save lives. But they also disrupt the invisible ecosystem inside you. Probiotics aren’t a cure-all, but when used correctly, they’re one of the few tools we have to protect your gut without compromising treatment. It’s not about avoiding antibiotics-it’s about giving your body the support it needs to recover.




Christina Widodo
January 14, 2026 at 11:37
I took Culturelle with my last round of amoxicillin and honestly? No more midnight bathroom runs. I used to dread antibiotics because I’d be stuck to the toilet for days. This time? I went hiking on day 4. Game changer.
Also, I started them day one like the article said-didn’t wait till I felt sick. That’s the key.
PS: I bought the refrigerated bottle. The cheap one from Walmart? Total waste.