When you pick up a prescription, you might see two options: the brand-name pill you’ve heard of, or a cheaper generic version. Many people wonder - does switching to a generic change how your drugs interact with each other? The short answer: no. The risk of drug interactions is essentially the same for generic and brand-name medications. But why does this confusion keep popping up? And when should you really worry?
What Makes a Drug Generic?
A generic drug isn’t a copy. It’s the same medicine, legally required to have the exact same active ingredient, strength, dosage form, and how it’s taken (like pill, injection, or inhaler) as the brand-name version. The U.S. Food and Drug Administration (FDA) doesn’t just approve generics based on a label check. They demand proof - called bioequivalence - that the generic delivers the same amount of the active drug into your bloodstream at the same rate as the brand. That means your body absorbs it the same way.Here’s the technical part: for most drugs, the FDA requires the generic’s absorption to fall within 80% to 125% of the brand’s. That sounds wide, but in practice, most generics are within 5% of the original. This range exists because human bodies vary. One person might absorb a drug slightly faster than another. The goal isn’t perfection - it’s therapeutic sameness.
What’s different? The inactive ingredients. Things like fillers, dyes, or preservatives. These don’t affect how the drug works. But they can matter in rare cases - like if you’re allergic to lactose, and a generic version uses it as a filler while the brand doesn’t. That’s not a drug interaction. That’s an allergy. And pharmacists can check for that.
Drug Interactions Depend on the Active Ingredient
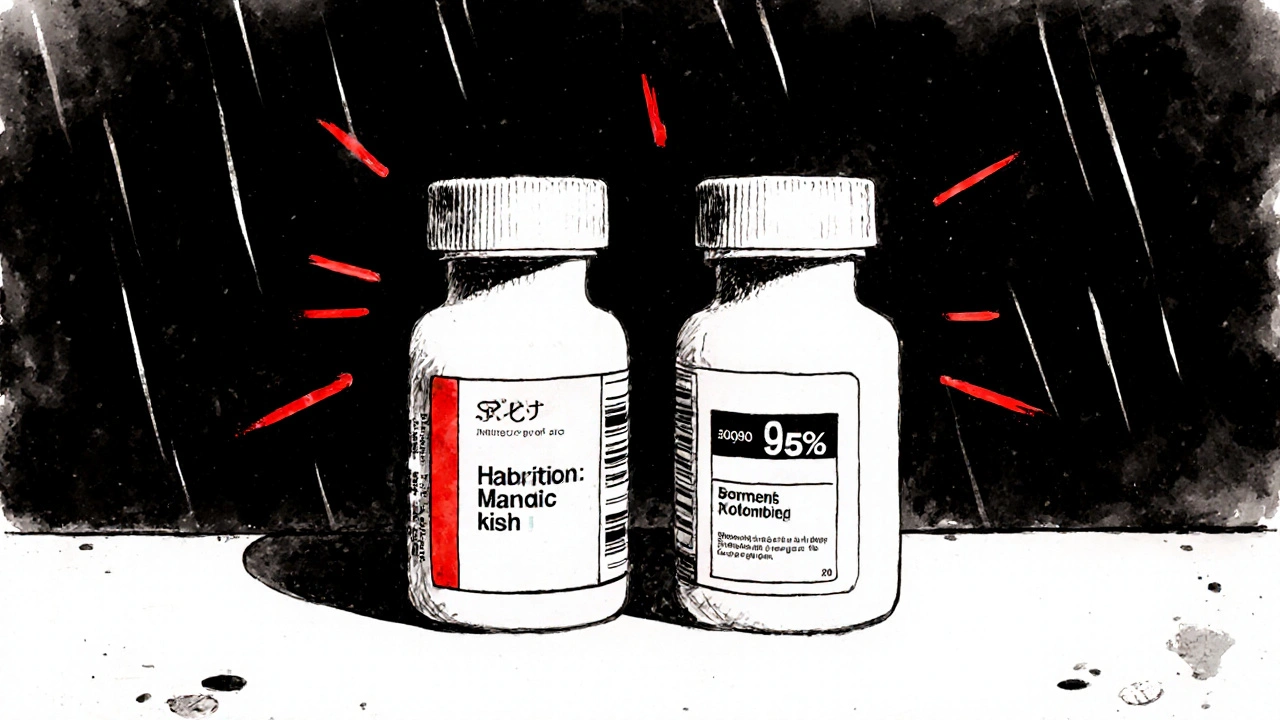
Drug interactions happen because of how the active chemical in a medicine behaves in your body. If you’re taking warfarin, for example, the risk of bleeding with certain antibiotics or supplements comes from warfarin itself - not whether it’s called Coumadin or just warfarin. The same goes for statins, antidepressants, or seizure meds. The active molecule is what interacts with your liver enzymes, your kidneys, or other drugs in your system.Studies back this up. A major 2020 study in Scientific Reports looked at 17 cardiovascular drugs and followed over 100,000 patients. The results? People taking generic versions had fewer heart attacks, strokes, and deaths than those on brand-name versions. Not because generics are stronger - but because more people could afford to take them consistently. The interaction risks? Exactly the same.
The FDA’s own adverse event database, FAERS, shows no meaningful difference in interaction-related reports between brand and generic drugs. From 2015 to 2020, 0.78% of brand-name users reported interaction issues. For generics, it was 0.82%. That difference? Statistically meaningless. Like flipping a coin and getting heads 51 times out of 100.
Why Do People Think Generics Are Different?
It’s not just about science. It’s about perception.When someone switches from a brand-name drug to a generic and suddenly feels different - more tired, dizzy, or nauseous - they often blame the generic. But in many cases, it’s the nocebo effect: expecting something to go wrong makes you notice normal side effects more. WebMD’s data shows complaints spike in the first three months after a new generic hits the market, then drop back to normal. Why? People stop expecting trouble.
Reddit threads and online forums are full of stories like: “I switched to generic zolpidem and now I’m extra drowsy with my antidepressant.” But when you dig deeper, the active ingredient - zolpidem - hasn’t changed. The interaction risk between zolpidem and sertraline was always there. The brand version just hid it from your awareness.
Also, there’s a psychological comfort in brand names. You’ve seen the ads. You trust the logo. But that doesn’t make the medicine safer. It just makes you feel safer.
When You Should Be Careful
There are exceptions. For drugs with a narrow therapeutic index - meaning the difference between a helpful dose and a dangerous one is tiny - even small changes in absorption can matter. Think warfarin, lithium, thyroid meds, or some anti-seizure drugs.For these, the FDA requires tighter bioequivalence standards: 90% to 111% instead of 80% to 125%. And even then, studies show no increase in adverse events when switching between generics or from brand to generic.
Still, if you’re on one of these drugs, consistency matters. Don’t switch between different generic brands every month. Stick with one manufacturer’s version. Why? Because while each generic meets FDA standards, two different generics might have slightly different release patterns. Not enough to be unsafe - but enough that your doctor might want to monitor your levels if you switch back and forth.
Pharmacists at major hospitals like UCSF now check both active and inactive ingredients when patients report new side effects after a switch. It’s not because generics are riskier. It’s because they’re thorough. They know that rare excipient issues - like a filler causing stomach upset - can be mistaken for a drug interaction.
What Experts Say
Dr. Aaron Kesselheim, a leading drug safety researcher at Harvard, put it simply: “The vast majority of evidence suggests that generic drugs are therapeutically equivalent to their brand-name counterparts, including regarding drug interaction profiles.”The FDA’s Center for Drug Evaluation and Research says the same: inactive ingredients don’t change how the active ingredient interacts with other drugs. The American College of Clinical Pharmacology agrees. Their 2020 position statement says bioequivalent drugs should have equivalent interaction risks.
But even experts acknowledge one thing: if you’re on multiple medications and have a complex condition, switching between different generic brands might be something to track. Not because it’s dangerous - but because your body might react to subtle changes in how the drug is released. That’s why your doctor might ask you to stay on the same generic version.
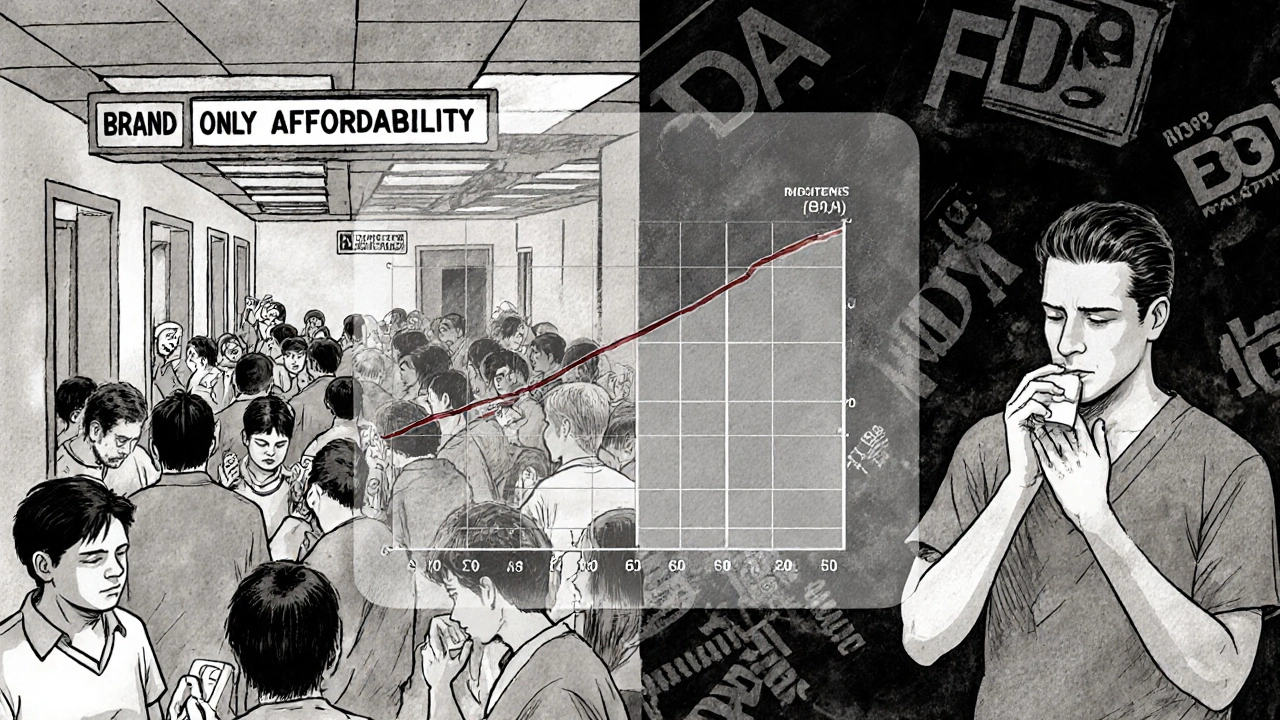
Real-World Impact: Cost and Compliance
Here’s the real danger: not taking your medicine because it’s too expensive.Generics make up 90% of all prescriptions in the U.S. but cost only 23% of what brand-name drugs do. That’s over $1.68 trillion saved in the last decade. That’s not just money. It’s lives. People who can’t afford their blood pressure pills skip doses. People who can’t afford their antidepressants stop taking them. That’s when interactions become dangerous - not because of the pill’s name, but because they’re not taking anything at all.
Studies show that patients on generics are more likely to stick with their treatment. And better adherence means fewer hospital visits, fewer complications, and fewer dangerous drug interactions caused by inconsistent dosing.
What You Should Do
- Don’t refuse a generic because you think it’s riskier. The science says otherwise.
- If you switch from brand to generic and feel different, talk to your pharmacist. Ask: “Could this be the filler? Or is it the drug itself?”
- If you’re on a narrow therapeutic index drug, ask your doctor if you should stick with one generic manufacturer.
- Always tell your pharmacist about every medication, supplement, and over-the-counter product you take - brand or generic.
- Don’t switch between different generic brands unless your doctor or pharmacist says it’s safe.
The bottom line: the name on the pill doesn’t change how your body handles it. What matters is the active ingredient. And that’s identical. The risk of drug interactions comes from what the drug is - not who made it.
What’s Changing Now
The FDA is investing $24 million through 2026 to study how multiple generic versions of the same drug might behave differently in real-world use. They’re using advanced testing and real patient data to make sure even the smallest differences are understood. But the goal isn’t to scare you. It’s to make sure the system stays safe as more generics flood the market.By 2028, nearly 8 out of 10 drugs coming off patent will have multiple generic makers. That’s good news for prices. And with better monitoring, it’s good news for safety too.



Scott McKenzie
November 28, 2025 at 23:09
Just switched my statin to generic last month and didn’t even notice. My BP’s better too. 🤓💊