Planning for a baby isn’t just about getting pregnant-it’s about making sure your body is ready to support a healthy pregnancy from day one. And one of the most important steps you can take? Reviewing every medication you’re taking before conception. Many women don’t realize that the critical window for fetal development begins before they even know they’re pregnant. By the time a missed period signals pregnancy, the baby’s heart, brain, and spine have already started forming. That’s why a preconception medication plan isn’t optional-it’s essential.
Why Timing Matters More Than You Think
Most major birth defects happen between weeks 3 and 8 of pregnancy. That’s before many women take a pregnancy test. If you’re taking a medication that can interfere with fetal development, waiting until you’re pregnant to make changes could mean missing that window entirely. The American College of Obstetricians and Gynecologists (ACOG) says 45% of pregnancies in the U.S. are unintended. That means nearly half of all women are exposed to medications during this critical period without even knowing it. This isn’t theoretical. Studies show that women who get a preconception medication review have 28% fewer major birth defects than those who don’t. The difference isn’t just in risk-it’s in outcomes. A baby born without a heart defect, neural tube defect, or cleft palate changes everything for a family.What Medications to Watch Out For
Not all medications are dangerous during pregnancy-but some are. The key is knowing which ones and what to do about them.- Valproic acid (used for seizures and bipolar disorder): Increases the risk of major congenital malformations to nearly 11%. It can also affect cognitive development. Switching to lamotrigine or levetiracetam before conception reduces that risk dramatically.
- Lithium (for bipolar disorder): Linked to a rare but serious heart defect called Ebstein’s anomaly. If you’re on lithium, your doctor should help you transition to a safer alternative at least 3-6 months before trying to conceive.
- Methotrexate (for autoimmune diseases like rheumatoid arthritis or psoriasis): A known teratogen. Even small doses can cause miscarriage or severe birth defects. You need at least 3 months-sometimes longer-after your last dose before attempting pregnancy.
- Isotretinoin (Accutane for acne): One of the most dangerous drugs in pregnancy. It can cause brain, heart, and facial defects. The iPLEDGE program requires 1 month of contraception after stopping it-but many women need longer. Don’t rely on memory; use a calendar and confirm with your dermatologist.
- Warfarin (blood thinner): Crosses the placenta and can cause fetal warfarin syndrome. If you’re on it for a clotting disorder, you’ll need to switch to low-molecular-weight heparin (like Lovenox) before conception. This is safe during pregnancy because it doesn’t cross the placenta.
- Topiramate (for seizures or migraines): Raises the risk of oral clefts from 0.36% to 1.4%. If you’re on it, your neurologist should consider switching you to a lower-risk option.
The One Supplement Everyone Needs
Folic acid isn’t just a suggestion-it’s a medical necessity. The World Health Organization recommends 400 micrograms daily for all women of reproductive age, regardless of whether they’re trying to get pregnant. Why? Because neural tube defects-like spina bifida and anencephaly-can happen before you know you’re pregnant. But if you have certain conditions, you need more:- General population: 400-800 mcg daily
- History of neural tube defect in previous pregnancy: 4,000-5,000 mcg daily (4-5 mg)
- On anticonvulsants like valproic acid or carbamazepine: 4,000-5,000 mcg daily
- Diabetes or obesity (BMI ≥30): 4,000-5,000 mcg daily

Chronic Conditions and Medication Adjustments
If you have a chronic illness, your preconception plan needs to be even more detailed.Thyroid Disease
Hypothyroidism during early pregnancy increases miscarriage risk by 60%. Your TSH (thyroid-stimulating hormone) should be under 2.5 mIU/L before conception. If you’re on levothyroxine, your dose may need to increase by 30% as soon as you confirm pregnancy. Don’t wait-get your levels checked 3-6 months before you start trying.Autoimmune Diseases
Drugs like cyclophosphamide and leflunomide are off-limits before and during pregnancy. But not all are dangerous. Sulfasalazine and hydroxychloroquine are generally safe and can be continued. Work with a rheumatologist to find the safest combo for your condition. Stopping your meds cold turkey can cause a flare-and a flare during pregnancy is riskier than staying on safe drugs.HIV
If you’re living with HIV, your goal is to have an undetectable viral load before conception. The American Society for Reproductive Medicine says keeping your viral load under 50 copies/mL reduces transmission risk to less than 1%. Some antiretrovirals are safer than others. Your infectious disease specialist should help you switch to a pregnancy-friendly regimen at least 3 months ahead of time.What to Do in the 6-Month Window
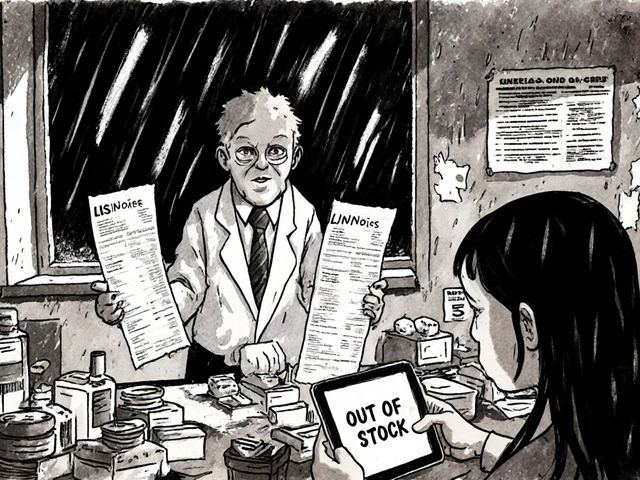
You don’t need to figure this out alone. A structured 6-month plan gives you time to make changes safely.- Month 1-2: List every medication, supplement, and herbal product you take. Include over-the-counter drugs like ibuprofen, antacids, and sleep aids. Bring this list to your primary care doctor or OB/GYN.
- Month 3: Schedule appointments with specialists: neurologist, rheumatologist, endocrinologist, or psychiatrist if needed. They’ll help adjust your meds.
- Month 4: Start high-dose folic acid if you’re in a high-risk group. Get your thyroid levels checked. Confirm your contraception method is effective-some seizure meds reduce the effectiveness of birth control pills.
- Month 5: Complete any medication switches. Confirm your new meds are stable and you’re not having side effects.
- Month 6: Get a final review. Make sure your lab work is normal. Discuss your plan with your partner. You’re ready.
What About Supplements and Herbal Remedies?
Just because something is “natural” doesn’t mean it’s safe. St. John’s wort can interfere with antidepressants and birth control. Black cohosh may stimulate uterine contractions. Dong quai can thin the blood. Even common herbs like echinacea or ginseng have limited safety data in pregnancy. Your doctor needs to know everything you’re taking. No judgment. No shame. Just facts. The goal is safety-not perfection.
Why This Isn’t Happening More Often
You’d think this would be routine. But here’s the truth: only 38% of women with chronic conditions get a preconception medication review, according to CDC data. Why?- Doctors don’t ask. Most OB/GYNs don’t bring it up unless the patient does.
- Time constraints. A 15-minute appointment isn’t enough to review 10 medications.
- Fragmented care. Your rheumatologist doesn’t talk to your OB. Your pharmacist doesn’t know you’re trying to get pregnant.
What to Do If You’re Already Pregnant
If you’re already pregnant and haven’t reviewed your meds, don’t panic. But don’t wait either. Call your doctor today. Many changes can still be made safely in the first trimester. And if you’re on something dangerous, your provider can monitor your baby closely with targeted ultrasounds and blood tests. The goal isn’t guilt. It’s action. Even if you’re 6 weeks along, getting your meds right now can still make a difference.Final Thought: This Is Prevention, Not Reaction
Pregnancy isn’t a time to fix problems-it’s a time to protect. The best time to manage your health is before you conceive. A medication plan isn’t about giving up your treatments. It’s about finding safer ways to stay healthy-for you and your future baby. If you’re taking any prescription or over-the-counter meds, and you’re thinking about having a child-start today. Make that list. Call your doctor. Ask the questions. Your future child will thank you.Do I need to stop all my medications before getting pregnant?
No. Many medications are safe during pregnancy, and stopping them abruptly can be more dangerous than continuing them. The goal is to switch to safer alternatives when needed, not to stop everything. For example, if you’re on warfarin, you’ll switch to heparin-not stop blood thinners entirely. Always work with your doctor to make changes safely.
How long before conception should I start planning?
At least 3-6 months. Some medications, like methotrexate or isotretinoin, require 3-6 months to fully clear your system. Others, like folic acid or thyroid meds, need time to stabilize your levels. Starting early gives you room to adjust without rushing.
Can I take over-the-counter pain relievers like ibuprofen before pregnancy?
Occasional use is fine, but regular use isn’t recommended. Ibuprofen and other NSAIDs can affect ovulation and reduce fertility. They’re also linked to higher risks in early pregnancy. Switch to acetaminophen (Tylenol) as your go-to pain reliever when trying to conceive.
What if I’m on birth control and want to get pregnant?
Stop your birth control when you’re ready. Most women resume ovulation within a few weeks. If you’re on a hormonal IUD or implant, your doctor can remove it. If you’re on pills, patches, or rings, stop them and start tracking your cycle. You can begin trying immediately after stopping-no waiting period is needed.
Is it safe to take vitamins or supplements before pregnancy?
Yes-especially folic acid. But avoid high-dose vitamin A (retinol), as too much can cause birth defects. Stick to prenatal vitamins with 400-800 mcg of folic acid. Avoid herbal supplements unless your doctor approves them. More isn’t always better.
What if my doctor doesn’t know much about preconception meds?
Ask for a referral to a maternal-fetal medicine specialist or a pharmacist who specializes in pregnancy. Many hospitals have teratogen information services (like MotherToBaby) that offer free, expert advice. You can also visit MotherToBaby.org for up-to-date, science-backed guidance on medications and pregnancy.



Elen Pihlap
January 7, 2026 at 12:44
this is so important i wish someone had told me this before i got pregnant with my first kid and i was on that mood stabilizer and didn't know it could mess up the baby
now my son has mild developmental delays and i blame myself every day