When you pick up a prescription, you might see a different name on the bottle than what your doctor wrote. Instead of BrandName, it says the chemical name - like atorvastatin instead of Lipitor. That’s a generic drug. And for most people, it works just fine. But a lot of patients swear they feel worse after switching. Headaches. Fatigue. Anxiety. Even worse, some report their blood pressure or thyroid levels going haywire. So, are generics less safe? Or is something else going on?
What Does ‘Bioequivalent’ Really Mean?
The FDA says generics must be bioequivalent to the brand-name version. That means the active ingredient - the part that actually treats your condition - must enter your bloodstream at the same rate and in the same amount. The allowed range? Between 80% and 125% of the brand’s absorption. That’s a 45% window. For most drugs, that’s fine. Your body can handle it. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or phenytoin - even small changes can matter. A 10% dip in absorption might mean your INR drops too low. A 10% spike could push you into bleeding risk. That’s why doctors sometimes write “Dispense as Written” on prescriptions for these drugs. It’s not about distrust. It’s about consistency. If you’ve been stable on one brand of levothyroxine for years, switching to a different generic manufacturer might nudge your thyroid levels out of range. Not because the generic is bad. But because each manufacturer uses slightly different fillers, binders, or coatings. Those inactive ingredients don’t treat your condition. But they can change how fast the drug dissolves - and that’s enough to throw off sensitive systems.Are Generics Actually Less Safe? The Data Says Mostly No
A major 2018 study in PLOS Medicine looked at 38 clinical trials involving heart drugs, thyroid meds, and antidepressants. The conclusion? No meaningful difference in safety or effectiveness between generics and brand-name versions. Patients on generic versions had the same rates of heart attacks, hospitalizations, and strokes. That’s reassuring. But then you look at the adverse event reports. A 2018 NIH analysis of over 27,000 reports found that generics showed higher numbers of side effect reports - but so did authorized generics (AGs), which are made by the same company as the brand. That’s a clue. If the same company makes both versions, and the generic still gets more reports, it’s probably not about manufacturing quality. It’s about perception.The Nocebo Effect: When Expectations Make You Sick
Here’s a weird but well-documented fact: people who think they’re taking a generic report more side effects - even when they’re not. A 2012 study gave people identical placebo pills. One group was told they were a brand-name drug. The other was told they were a generic. The “generic” group reported more headaches, dizziness, and nausea. Same pills. Same dose. Just different labels. This isn’t just in labs. Real patients report changes after switching. One Reddit user wrote: “I switched from Wellbutrin XL to generic bupropion and started having panic attacks at 3 a.m. every night.” Another said their cholesterol shot up after switching from Lipitor to atorvastatin. Doctors checked the levels - everything was within bioequivalence range. But the symptoms were real. The mind doesn’t distinguish between pharmacology and psychology here. If you’ve been told generics are “cheaper” or “not as good,” your brain starts looking for proof. You notice a headache. You remember you switched pills. Boom - causal link formed. It’s the nocebo effect in action. And it’s powerful.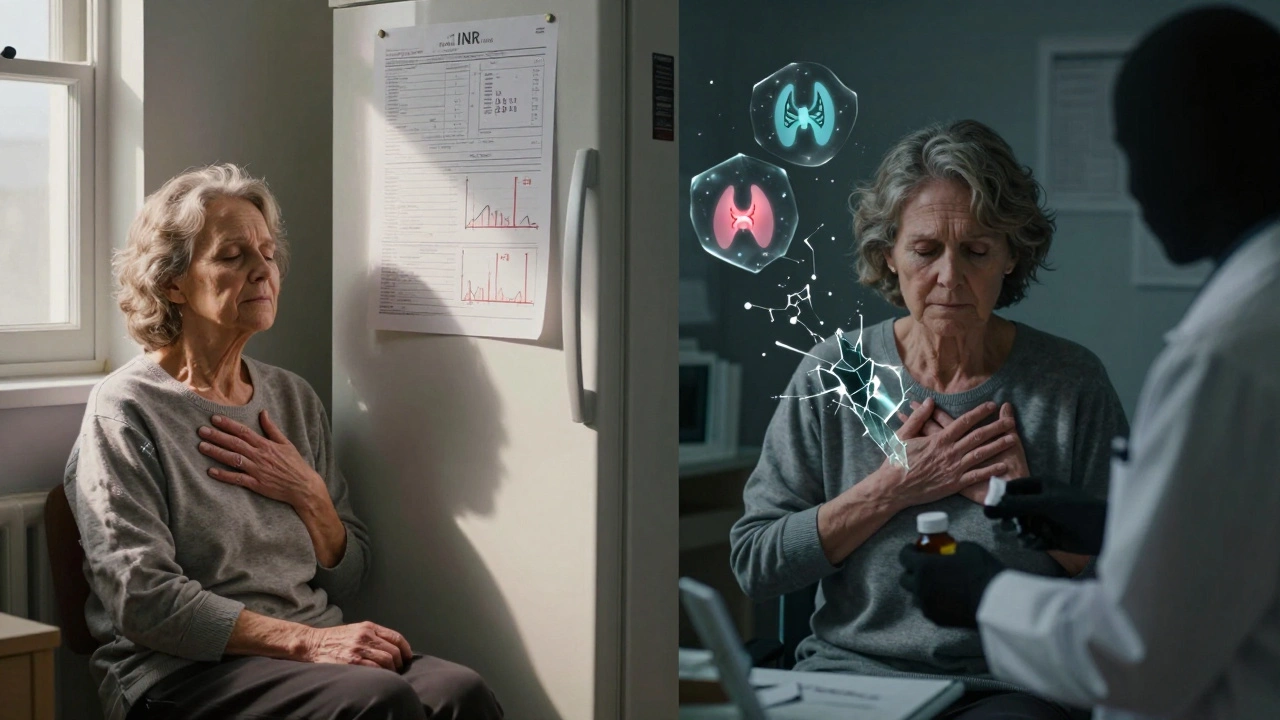
Manufacturing Matters - Especially Outside the U.S.
Not all generics are made the same. About 63% of generic drug factories are outside the U.S., mostly in India and China. A 2022 Ohio State University study found that generics made in India were linked to 54% more severe adverse events - including hospitalizations and deaths - compared to those made in the U.S. The difference? Mature drugs. The ones that’ve been on the market for 10+ years. Cheaper production. Less oversight. Lower profit margins. Some manufacturers cut corners. The FDA inspects foreign plants more now than ever - 317 in 2022, up from 42 in 2010. But 12% of foreign facilities still get flagged for serious violations. That’s not nothing. If you’re on a generic that’s been on the market for years and suddenly feels off, it might not be your brain. It might be the pill.Who’s Most at Risk?
Not everyone needs to worry. But some people should be extra careful:- People on warfarin - tiny changes in absorption can cause clots or bleeds.
- Patients on levothyroxine - even 5% variation can throw off thyroid function.
- Those on anti-seizure drugs like phenytoin or carbamazepine - narrow window, high risk.
- Older adults on multiple meds - more chances for interaction or absorption changes.
- Anyone who noticed a change after switching - even if labs look fine.

What Should You Do?
Here’s the practical advice:- Don’t panic. For 90% of people, generics are perfectly safe.
- If you feel worse after switching, don’t assume it’s “all in your head.” Track your symptoms - when they started, how bad they are, what else changed.
- Ask your pharmacist: “Is this the same manufacturer as before?” Sometimes the same generic, from the same company, works fine. It’s switching between manufacturers that causes issues.
- For high-risk drugs, ask your doctor to write “Dispense as Written.” It might cost more, but stability matters more than savings.
- Use the FDA’s Orange Book (online) to check which generics are AB-rated. That means they’re approved as interchangeable.
- If you’re on a generic that’s been on the market for over 10 years and you’re having problems, ask if a newer version exists. Older generics sometimes use outdated manufacturing methods.
What’s Changing Now?
The FDA is getting smarter. Their Sentinel Initiative now tracks 300 million patient records to spot adverse event patterns in real time. They’re also pushing for more post-market studies on complex generics - things like inhalers, creams, and extended-release pills. These are harder to copy exactly. A 2023 study in JAMA Network Open found that genetic differences matter too. People with certain liver enzyme variations (like CYP2D6 poor metabolizers) had 2.3 times more side effects with generic venlafaxine. That’s the future: personalized generics based on your DNA. For now, the consensus is clear: generics save billions and work for nearly everyone. But they’re not magic. They’re medicine. And like any medicine, they can behave differently in different people.Frequently Asked Questions
Are generic drugs less effective than brand-name drugs?
No, for the vast majority of medications, generics are just as effective. The FDA requires them to deliver the same active ingredient in the same amount and at the same rate as the brand-name version. Studies involving hundreds of thousands of patients show no difference in outcomes for conditions like high blood pressure, cholesterol, or depression. The only exceptions are drugs with a narrow therapeutic index - like warfarin or levothyroxine - where even small changes in absorption can matter.
Why do some people feel worse on generic medications?
There are two main reasons. First, the inactive ingredients - like fillers, dyes, or coatings - can vary between manufacturers. These don’t treat your condition, but they can affect how fast the drug dissolves, which matters for sensitive patients. Second, the nocebo effect plays a big role. If you believe generics are inferior, your brain can amplify normal sensations into side effects. Studies show people report more headaches or nausea when told they’re taking a generic - even when it’s a placebo.
Should I avoid generics made in India or China?
Not necessarily, but be aware. A 2022 study found that generics made in India were linked to 54% more severe adverse events compared to U.S.-made versions - especially older drugs that have been on the market for over a decade. This isn’t because all Indian-made drugs are unsafe. It’s because some manufacturers cut costs, and oversight can be inconsistent. The FDA inspects foreign plants, but 12% still get flagged for serious issues. If you’re on a long-term medication and notice new side effects, ask your pharmacist where it’s made.
Can I switch back to the brand-name drug if I don’t feel right?
Yes, absolutely. If you feel worse after switching, talk to your doctor. You can ask them to write “Dispense as Written” on your prescription, which stops the pharmacy from substituting. Some insurance plans require prior authorization for brand-name drugs, but if you can document a clear change in symptoms after switching, they often approve it. Your health matters more than cost savings.
How do I know if my generic is safe?
Check the FDA’s Orange Book to see if your generic is rated AB - meaning it’s approved as interchangeable. Ask your pharmacist which manufacturer makes your version. If you’re on a high-risk drug, stick with the same manufacturer unless your doctor advises otherwise. Keep a symptom journal: note when you started the new generic and what changed. That data helps your doctor decide if it’s the pill or something else.






sean whitfield
December 5, 2025 at 23:54
Generics are just Big Pharma’s way of making you sick so they can sell you the brand name again later. 😏