What Are Monoclonal Antibody Biosimilars?
Monoclonal antibody biosimilars are not generics. They’re not copies like the cheap pills you get for high blood pressure or cholesterol. These are complex biological medicines made from living cells-usually engineered human or animal cells-that mimic the structure and function of an already-approved original drug, called the reference product. Think of them as identical twins, not clones. They’re designed to work the same way, but because they’re made from proteins that are 150,000 daltons in size (about six times heavier than insulin), tiny differences in how they’re made can show up in how they behave. That’s why regulators don’t call them generics. They call them biosimilars.
The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) both require that biosimilars show no clinically meaningful differences in safety, purity, or effectiveness compared to the original. That means if your doctor prescribes a biosimilar for rheumatoid arthritis or breast cancer, you can expect the same results as the brand-name drug. But the cost? That’s where the big difference lies.
Why Biosimilars Matter
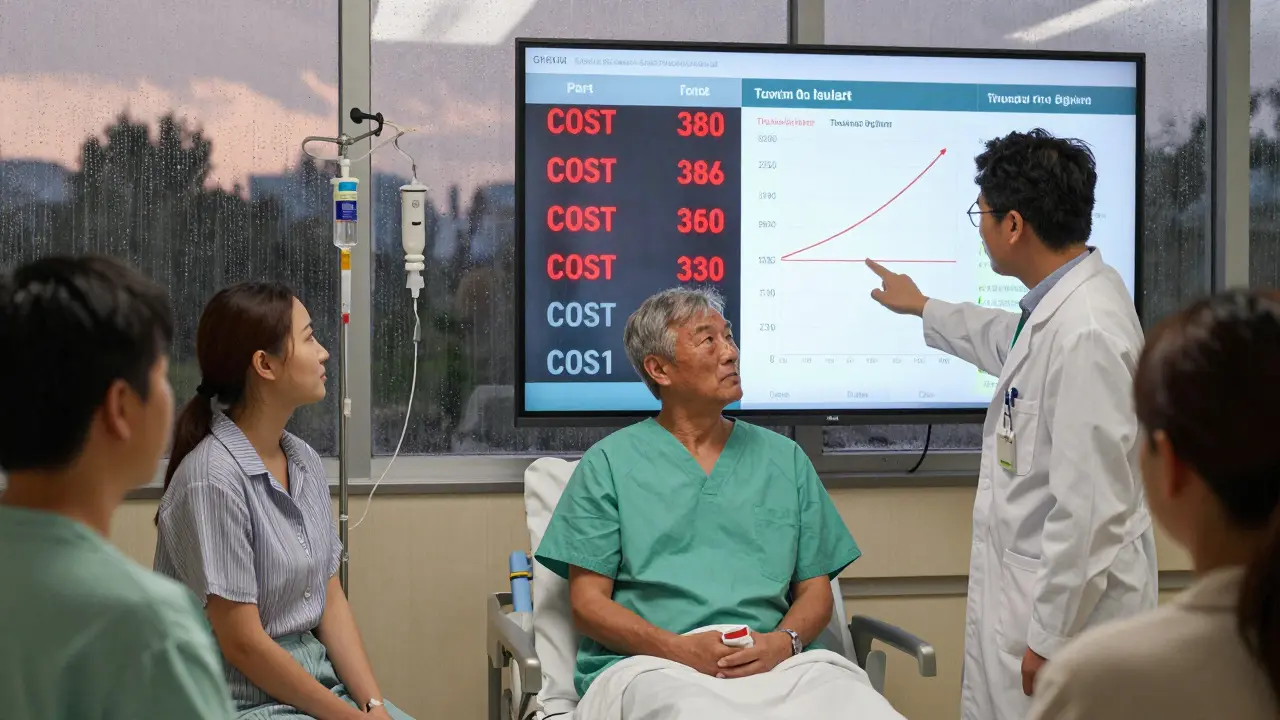
Monoclonal antibody drugs like Herceptin, Rituxan, and Avastin changed cancer care. But they also changed healthcare budgets. A single course of Herceptin used to cost over $70,000 in the U.S. before biosimilars arrived. Now, with multiple biosimilars approved, prices have dropped by 30% to 50% in many cases. That’s not just savings for insurance companies-it’s access for patients who couldn’t afford treatment before.
A 2022 study in JAMA Oncology tracked 1,247 patients switching from Rituxan to its biosimilar Truxima across 15 U.S. cancer centers. The results? No drop in effectiveness. No spike in side effects. And a 28% reduction in cost per treatment cycle. That’s real money. And it’s happening across dozens of hospitals.
These savings add up fast. Industry analysts at Evaluate Pharma predict biosimilar monoclonal antibodies will save the U.S. healthcare system $250 billion between 2023 and 2028. Bevacizumab, trastuzumab, and rituximab biosimilars alone will make up 78% of those savings.
Approved Monoclonal Antibody Biosimilars and Their Uses
Here’s what’s actually on the market in the U.S. as of 2026:
- Bevacizumab biosimilars (Avastin copies): Mvasi, Zirabev, Alymsys, Vegzelma, Avzivi, Jobevne. Used for colorectal, lung, and brain cancers.
- Rituximab biosimilars (Rituxan copies): Truxima, Ruxience, Riabni. Used for non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and autoimmune diseases like rheumatoid arthritis.
- Trastuzumab biosimilars (Herceptin copies): Ogivri, Herzuma, Ontruzant, Trazimera, Kanjinti, Hercessi. Used for HER2-positive breast and stomach cancers.
- Infliximab biosimilars (Remicade copies): Inflectra, Renflexis, Avsola, Ixifi, Remsima, and the first FDA-interchangeable one, Inflectra, approved in 2023. Used for Crohn’s disease, ulcerative colitis, psoriasis, and ankylosing spondylitis.
- Adalimumab biosimilars (Humira copies): Amjevita, Cyltezo, Hyrimoz, Hadlima, and others. Used for arthritis, psoriasis, and inflammatory bowel disease.
There are now six approved trastuzumab biosimilars in the U.S. alone. That’s more than the original manufacturer ever had on the market at once. For patients, that means more options, more competition, and lower prices.
How Are They Different From Generics?
Generic pills are simple. You take a chemical formula, replicate it exactly, and you’ve got a generic. Aspirin is aspirin. Metformin is metformin. No matter who makes it, the molecule is identical.
Monoclonal antibodies? Not even close. They’re made by living cells in huge bioreactors. Even the same company can’t make two batches that are exactly the same. Tiny changes in sugar chains (glycosylation), protein folding, or impurities can happen naturally during production. That’s why regulators require biosimilar makers to run over 100 analytical tests-mass spectrometry, protein sequencing, cell-based assays-to prove similarity down to the molecular level.
And that’s not all. They also need to show the biosimilar works the same in clinical trials. Usually, they test it in one sensitive condition-like rheumatoid arthritis for infliximab-to prove it’s just as safe and effective as the original. Then, they get approval for all other uses the original drug has.
Interchangeable Biosimilars: What Does That Mean?
Not all biosimilars are created equal when it comes to switching. Most require a doctor’s approval to switch from the original to the biosimilar. But some are now designated as interchangeable.
That’s a special FDA status. It means a pharmacist can substitute the biosimilar for the original without asking the doctor-just like a generic. The first monoclonal antibody biosimilar to get this status was Inflectra (infliximab) in July 2023. That’s a big deal. It removes a major barrier to adoption.
But here’s the catch: only a few interchangeable biosimilars exist right now. Most still need a prescriber’s OK. That’s because proving interchangeability requires extra data: studies showing multiple switches back and forth don’t increase risks. It’s harder to prove, so fewer companies have done it.
Real-World Safety: Are They Safe?
Some patients worry: if it’s not the same drug, could it cause new side effects?
That’s a fair question. But data says no. The EMA reviewed over 1.2 million patient-years of exposure to monoclonal antibody biosimilars from 2010 to 2021. They found only 12 cases of unexpected immune reactions. That’s a rate of 0.001%-exactly the same as the reference products.
One concern in the past was about a rare allergic reaction to cetuximab, linked to a sugar molecule called alpha-gal. That wasn’t caused by the biosimilar-it was a feature of the original drug. The same risk exists with both. Biosimilars don’t create new risks. They replicate the original’s profile, including its known side effects.
And because they’re newer, they’re monitored more closely. Every biosimilar has a special tracking system to catch any unusual patterns. That’s more oversight than the original drug ever had.

What’s Coming Next?
The pipeline is packed. As of late 2023, the FDA had 37 monoclonal antibody biosimilars under review. The biggest targets are:
- Humira (adalimumab): 14 biosimilars in development. Hyrimoz was the first U.S. approval in 2023.
- Keytruda (pembrolizumab): Six biosimilars in late-stage trials. This is huge-Keytruda is one of the most widely used cancer immunotherapies.
- Enbrel (etanercept): Already has multiple biosimilars, but more are coming.
And it’s not just single antibodies. Companies are working on biosimilars for more complex drugs: bispecific antibodies (which target two cancer markers at once) and antibody-drug conjugates (which deliver chemo directly to cancer cells). The EMA plans to release new guidelines for these by mid-2024.
Why Aren’t They Used More?
Despite the savings and safety data, adoption isn’t universal. Three big barriers hold back faster use:
- Patent lawsuits: Drugmakers fight biosimilar entry with dozens of legal challenges. On average, each monoclonal antibody biosimilar faces 14.7 patent disputes before it can launch.
- Doctor hesitation: A 2022 survey by the American Society of Clinical Oncology found only 58% of oncologists felt ‘very confident’ prescribing biosimilars. Many still think they’re ‘second-tier’ drugs.
- Pharmacy benefit manager rules: Insurance companies often block biosimilars by putting them on higher cost tiers or requiring prior authorization. Thirty-two percent of biosimilar launches are delayed or blocked by these policies.
Education is key. When doctors see real data-like the 28% cost drop with no loss in effectiveness-they change their minds. Hospitals that switched entire cancer units to biosimilars saw faster patient access and lower costs without a single safety issue.
The Future of Biosimilars
By 2027, monoclonal antibody biosimilars are expected to make up 35% of all biologic prescriptions in the U.S.-up from just 18% in 2022. Cancer treatments will account for 62% of that volume.
That means more patients will get life-saving treatments. More hospitals will save millions. More insurers will lower premiums. And more people will live longer-not because a new miracle drug was invented, but because a smarter, cheaper version of an old one finally got the chance to help.
Monoclonal antibody biosimilars aren’t the future. They’re here. And they’re working.
Are monoclonal antibody biosimilars safe?
Yes. Regulatory agencies like the FDA and EMA require biosimilars to prove no clinically meaningful differences in safety, purity, or effectiveness compared to the original drug. Studies tracking over 1.2 million patient-years of use show the rate of unexpected immune reactions is the same as the reference product-about 0.001%. Biosimilars don’t introduce new risks; they replicate the known profile of the original.
How are biosimilars different from generics?
Generics are exact chemical copies of small-molecule drugs like aspirin or metformin. Biosimilars are highly similar-but not identical-copies of complex biological drugs made from living cells. Monoclonal antibodies are large proteins with intricate structures that can’t be perfectly replicated. Biosimilars must undergo extensive testing to prove similarity, while generics only need to prove bioequivalence.
Can pharmacists substitute biosimilars for brand-name drugs?
Only if the biosimilar is designated as ‘interchangeable’ by the FDA. As of 2026, only a few monoclonal antibody biosimilars have this status, including Inflectra (infliximab). For non-interchangeable biosimilars, a doctor must specifically prescribe the biosimilar. Pharmacists cannot switch them automatically.
Which cancers are treated with monoclonal antibody biosimilars?
Biosimilars of bevacizumab (Avastin) treat colorectal, lung, and brain cancers. Trastuzumab (Herceptin) biosimilars treat HER2-positive breast and stomach cancers. Rituximab (Rituxan) biosimilars treat non-Hodgkin’s lymphoma and chronic lymphocytic leukemia. These are among the most common cancer treatments now available as biosimilars.
How much money do biosimilars save?
Biosimilars typically cost 30% to 50% less than the original drug. A 2022 study found switching from Rituxan to Truxima saved 28% per treatment cycle. Industry analysts project biosimilar monoclonal antibodies will save the U.S. healthcare system $250 billion between 2023 and 2028, with bevacizumab, trastuzumab, and rituximab biosimilars accounting for 78% of those savings.



Donna Macaranas
February 1, 2026 at 15:17
This is actually really hopeful. I have a friend on trastuzumab and the cost was insane. Knowing there are cheaper options that work just as well? That’s a win for real people.
Thanks for laying this out so clearly.