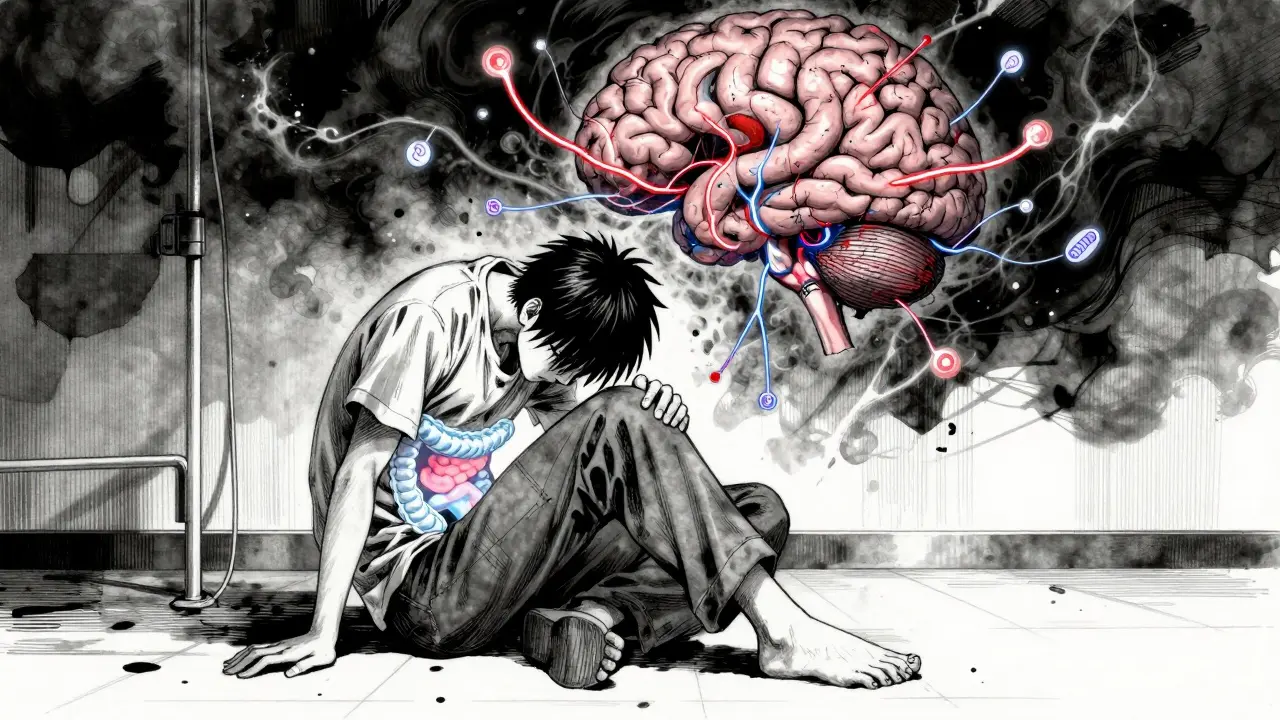
For millions of people, stomach pain, bloating, and unpredictable bowel changes aren’t just annoying-they’re life-limiting. If you’ve been told your symptoms are "just stress" or "all in your head," you’re not alone. But here’s the truth: your gut and brain aren’t just connected-they’re locked in a constant, invisible conversation. When that conversation goes wrong, irritable bowel syndrome follows.
What Really Causes IBS? It’s Not Just Your Digestion
For decades, doctors treated IBS like a simple gut problem-maybe your intestines were too slow, too fast, or too sensitive. But research since the 2010s has turned that idea upside down. Today, experts agree: IBS is a disorder of brain-gut-microbiome interactions. That means the issue isn’t just in your colon. It’s in how your brain reads signals from your gut, how your gut microbes talk to your nerves, and how stress and emotions hijack the whole system.
The gut-brain axis is a two-way highway. Your gut sends signals to your brain about hunger, fullness, pain, and discomfort. Your brain sends back instructions: slow down digestion, speed it up, release stress hormones, calm inflammation. In IBS, this system gets mixed up. Signals get distorted. Pain signals are amplified. Normal gut movements feel like cramps. Even the bacteria in your intestines-trillions of them-play a role by producing chemicals that influence your mood and nerve sensitivity.
The Science Behind the Symptoms
Brain scans of people with IBS show real, measurable differences. Those with diarrhea-predominant IBS (IBS-D) have thicker brain regions tied to sensing bodily sensations. Those with constipation-predominant IBS (IBS-C) show thinner areas linked to emotional regulation. These aren’t random changes-they’re patterns seen across hundreds of patients.
One of the biggest players? Serotonin. About 95% of your body’s serotonin is made in your gut, not your brain. In IBS-D, there’s too much of it-up to 60% higher than in people without IBS. That overstimulates the gut, speeding up movement and causing loose stools. In IBS-C, serotonin levels drop, slowing everything down. This isn’t just about mood-it’s about bowel control.
Immune activity in the gut is also off. People with IBS have lower levels of natural painkillers like β-endorphin in their intestines. That means even mild stretching from gas or stool feels like sharp pain. It’s like your body’s alarm system is stuck on high volume.
Why Anxiety and IBS Go Hand in Hand
It’s not coincidence that 60-70% of people with IBS also struggle with anxiety or depression. It’s biology. The same brain regions that process fear and stress-like the amygdala and anterior cingulate cortex-are the same ones that interpret gut signals. When you’re anxious, your brain becomes hyper-focused on bodily sensations. A normal gurgle becomes a warning sign. A slight cramp turns into a full-blown panic.
Stress doesn’t just make symptoms worse-it can trigger them. The HPA axis, your body’s main stress response system, releases cortisol when you’re under pressure. Too much cortisol changes gut motility, increases intestinal permeability (sometimes called "leaky gut"), and alters your microbiome. That’s why many people notice flare-ups before exams, during job stress, or after a breakup.

What Actually Works for Relief? Evidence-Based Strategies
Medications like antispasmodics or loperamide help some, but they often come with side effects-and don’t fix the root problem. The real breakthroughs are therapies that target the gut-brain axis directly.
Gut-directed hypnotherapy is one of the most powerful tools. In clinical trials, 70-80% of people saw major symptom improvement. It works by training the brain to ignore or reframe gut signals. Patients learn to visualize their gut as calm and steady. Unlike drugs, the benefits last-many stay symptom-free for years after just 6-12 sessions.
The low-FODMAP diet helps about 60% of people. FODMAPs are short-chain carbs found in onions, garlic, beans, apples, and wheat that ferment in the gut, pulling in water and creating gas. The diet isn’t about cutting out forever-it’s about identifying triggers. Most people start with a strict 4-6 week elimination, then slowly reintroduce foods to find their personal limits. It’s tough to stick to, but for many, it’s the difference between constant discomfort and normal life.
Probiotics aren’t all the same. The strain Bifidobacterium infantis 35624 has been shown in multiple studies to reduce bloating, pain, and bowel irregularity. Take 1 billion CFUs daily. Other probiotics? Most don’t help. Don’t waste money on random brands.
Emerging Treatments on the Horizon
Science is moving fast. In 2023, a new blood test called VisceralSense™ became available. It measures 12 microbial metabolites and serotonin ratios to predict which treatment will work best for you-personalized medicine for IBS. In phase III trials, a new drug called etrasimod reduced symptoms by over 50% in IBS-D patients, compared to just 31% with placebo.
Non-invasive devices like transcutaneous vagus nerve stimulators (tVNS) are being tested. These small patches, worn behind the ear, send gentle electrical pulses to the vagus nerve-the main communication line between gut and brain. Early results show 45-55% pain reduction. No pills. No side effects. Just a wearable device.

Why So Many People Struggle to Get Help
Most people wait 3 to 7 years before getting diagnosed. Why? Because many doctors still think IBS is a diagnosis of exclusion-"We ruled out everything else, so it must be IBS." That mindset leads to missed opportunities. You don’t need to rule out every disease first. If your symptoms match Rome IV criteria-abdominal pain at least once a week for three months, linked to bowel changes-you have IBS.
Cost and access are huge barriers. Gut-directed hypnotherapy costs $1,200-$2,500 out of pocket. Few insurance plans cover it. There’s only about one certified practitioner per 500,000 people in rural areas. The low-FODMAP diet requires a dietitian’s guidance, which isn’t always available.
And then there’s the stigma. People dismiss IBS as "just a sensitive stomach." But this isn’t weakness. It’s a real, measurable neurological condition. When patients understand the gut-brain connection, they’re 30% more likely to stick with treatment and 25% more likely to see improvement.
Where to Start Today
You don’t need to wait for a miracle drug. Start here:
- Learn the basics. Read the Rome IV criteria. Know what qualifies as IBS. This alone reduces anxiety.
- Try a low-FODMAP diet with a dietitian. Don’t guess-follow a structured plan.
- Look for a gut-directed hypnotherapist. Search the American Society of Clinical Hypnosis directory.
- Try Bifidobacterium infantis 35624 daily for 4 weeks. Track your symptoms.
- Reduce stress. Even 10 minutes of daily breathing exercises can calm your gut-brain axis.
IBS isn’t a life sentence. It’s a signal. Your body is trying to tell you something about how stress, food, and your nervous system are interacting. When you treat the gut-brain axis-not just the gut-you stop managing symptoms and start healing the system.
Is IBS just stress or anxiety?
No. While stress can worsen IBS, it’s not the cause. IBS is a real disorder of brain-gut communication with measurable biological changes-altered serotonin levels, immune activity, brain structure, and gut microbiome composition. Anxiety and depression often coexist because the same brain regions process both emotions and gut signals, but IBS exists independently.
Can IBS be cured?
There’s no permanent cure, but many people achieve long-term remission. Gut-directed hypnotherapy, the low-FODMAP diet, and targeted probiotics can reduce symptoms by 70% or more. For some, symptoms disappear for years. The goal isn’t to eliminate IBS entirely-it’s to regain control so it doesn’t control your life.
Do I need a colonoscopy to diagnose IBS?
Not always. The Rome IV criteria allow diagnosis based on symptoms alone if you’re under 50 and have no red flags like weight loss, bleeding, or family history of colon cancer. Colonoscopies are used to rule out other conditions, not to confirm IBS. Many doctors over-test. Ask: "Do my symptoms match IBS criteria?" before agreeing to invasive procedures.
Why do some foods trigger IBS but not others?
It’s about how your gut handles certain carbs called FODMAPs. These ferment quickly, pull water into the intestine, and produce gas. Everyone has different tolerance levels. Garlic might trigger you, but blueberries don’t. That’s why a personalized approach-like the low-FODMAP elimination and reintroduction process-is essential. It’s not about avoiding all "bad" foods. It’s about finding your unique triggers.
Are probiotics helpful for IBS?
Only specific strains. Bifidobacterium infantis 35624 is the only one with strong, repeated evidence for reducing pain, bloating, and bowel irregularity in IBS. Other probiotics-like those in yogurt or cheap supplements-often have no effect. Check the label. You need the exact strain and dose: 1 billion CFUs daily. Don’t waste money on random brands.
How long does gut-directed hypnotherapy take to work?
Most people see improvement within 4-6 sessions. A full course is typically 6-12 weekly sessions. Benefits often last for years after treatment ends. It’s not a quick fix-it’s a rewiring of how your brain responds to gut signals. Think of it like physical therapy for your nervous system.
What’s Next for IBS Treatment?
The future is personal. Researchers are building profiles of each person’s gut-brain axis-based on their microbiome, brain scans, serotonin levels, and stress response-to match them with the right treatment. The NIH’s $15 million Microbiome-Gut-Brain Consortium is already testing algorithms that predict whether someone will respond better to hypnotherapy, diet, or a new drug.
By 2030, IBS treatment will shift from trial-and-error to precision medicine. But you don’t have to wait. The tools to take control are here now. Understand your gut-brain axis. Use the evidence. Be your own advocate. Your symptoms aren’t random. They’re signals-and you have more power to heal than you think.





Paula Villete
December 23, 2025 at 17:20
Okay but have y’all noticed how every single "evidence-based" IBS solution is either expensive, hard to access, or requires you to become a full-time nutritionist? I get it-gut-brain axis, serotonin, microbiome… cool. But what if I work two jobs and can’t afford a dietitian or hypnotherapy? My gut doesn’t care about your clinical trials. It just wants me to eat something that doesn’t cost $12 a serving.
Also, I tried Bifidobacterium infantis 35624. Took it for 6 weeks. Felt like my intestines were slowly turning into a deflated balloon. Then I ate a bag of chips and everything came back worse. So… congrats? I guess science works… if you’re rich and have unlimited free time.