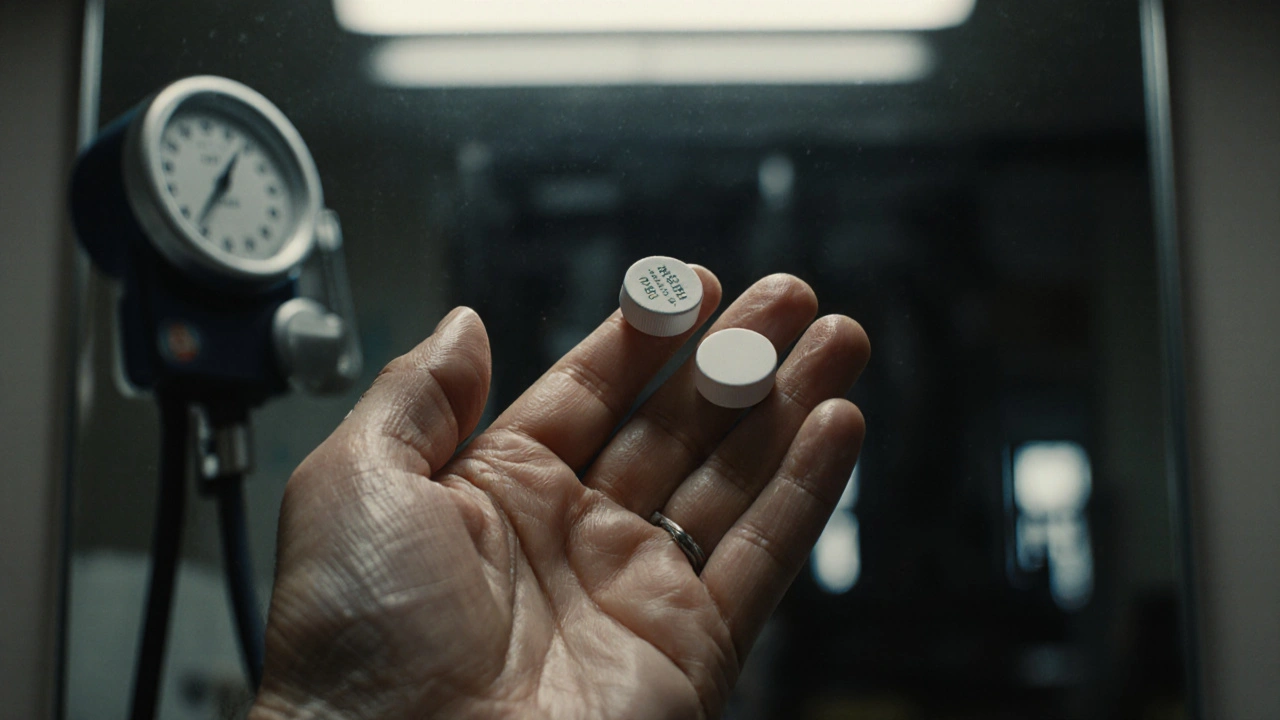
It’s supposed to be the same drug. Same active ingredient. Same price. So why does it sometimes feel like your generic medication just… doesn’t work?
You’re taking your blood thinner, your seizure medicine, or your transplant drug - the one your doctor prescribed, the one you’ve been on for months. But lately, you’re dizzy, your INR levels are all over the place, or your seizures are coming back. Your doctor says your condition is worsening. But what if it’s not your disease? What if it’s your pill?
Generic drugs are meant to be safe, affordable copies of brand-name medicines. In most cases, they are. But when they fail - when they don’t deliver the same effect - the consequences can be deadly. This isn’t rare. It’s not anecdotal. It’s happening right now, in hospitals and homes across the world, and it’s tied to a system that allows big gaps in quality control.
What Does "Bioequivalent" Really Mean?
The FDA says a generic drug must be "bioequivalent" to the brand-name version. That sounds solid. But here’s what that actually means: the amount of drug your body absorbs can be up to 20% less - or 25% more - than the original. That’s not a typo. For most medications, that range is fine. But for drugs with a narrow therapeutic index - like warfarin, phenytoin, digoxin, tacrolimus, or levothyroxine - that margin is dangerous.
These drugs don’t have room for error. Too little, and the disease comes back. Too much, and you bleed, have a seizure, or reject your transplant. A 15% drop in absorption might be harmless for an antibiotic. For warfarin, it could mean a stroke. A 20% spike? That could mean internal bleeding.
And here’s the catch: the FDA doesn’t test every batch. They test a few from a few factories. If those pass, the whole lot gets approved. But what if the next batch from the same factory has different fillers? Different manufacturing conditions? Different humidity control? That’s when things go wrong.
When the Pill Doesn’t Dissolve
It’s not just about how much active ingredient is in the pill. It’s about whether it dissolves at the right time, in the right place.
Take Concerta, the extended-release ADHD drug. The brand version releases medication slowly over 12 hours. One generic version dissolved in under an hour. Patients got a sudden spike of stimulant, followed by nothing. The result? Kids couldn’t focus in school. Parents thought the treatment had stopped working. The FDA eventually pulled that version from the market - but only after years of complaints.
The same thing happened with Budeprion XL, a generic version of Wellbutrin. Patients reported severe mood swings, anxiety, and even suicidal thoughts. The problem? The inactive ingredients - the ones you never see on the label - changed how the drug broke down in the stomach. The FDA withdrew approval in 2013. But many patients had already been switched to it, and some never fully recovered.
And it’s not just ADHD or depression drugs. In 2024, Glenmark recalled nearly 47 million potassium chloride tablets because they weren’t dissolving. Patients with heart conditions were getting no potassium at all - or getting crushed pills that burned their esophagus. That’s not a manufacturing error. That’s a systemic failure.
Chemical Degradation: The Silent Killer
Drugs don’t last forever. They break down. Heat, moisture, light - they all degrade the active ingredient. For a brand-name drug, the manufacturer runs months of stability tests to prove the pill stays effective until the expiration date.
But for generics? Some manufacturers cut corners. One study found that pills from the same blister pack had wildly different amounts of active ingredient - some contained only 72% of what was labeled. Others had over 112%. That’s not a typo. That’s actual lab data from TBIJ investigators.
For chemotherapy drugs, this isn’t just risky - it’s criminal. In cases of breast and ovarian cancer, patients were given generics that contained so little active ingredient that the treatment had no effect. Others got too much - leading to organ damage, severe vomiting, or death. One oncologist told investigators: "Giving them to patients would be as good as doing nothing."
Hydrolysis. Oxidation. Photolysis. These are technical terms. But here’s what they mean in real life: a pill stored in a hot warehouse in India, shipped through a humid port in Brazil, sitting on a shelf in a pharmacy in Australia - and then given to a patient who’s already weak from cancer. The drug inside? It’s half-dead before it’s swallowed.

Who’s Responsible When a Generic Fails?
When a patient has a bad reaction, who do you blame? The pharmacist who filled the prescription? The doctor who switched to generic? The manufacturer in China or India? The distributor? The Pharmacy Benefit Manager (PBM) that pushed the cheapest option?
It’s almost never anyone’s fault - because no one is held accountable.
Pharmacists are told to substitute generics unless the doctor says "do not substitute." They don’t know which factory made the pill. They don’t know if it passed stability tests. They don’t even know if the batch they’re holding has been recalled.
Doctors assume the generic is safe. They trust the FDA. But the FDA’s approval process is based on averages, not individual batches. And once a generic is on the market, there’s little follow-up. No one is watching the shelves.
Meanwhile, middlemen - PBMs - profit from switching patients to the cheapest generic, even if it’s the one with the highest failure rate. They get kickbacks. Patients get sicker.
What You Can Do - Before It’s Too Late
You can’t control the supply chain. But you can protect yourself.
- Know your drug’s therapeutic index. If you’re on warfarin, digoxin, phenytoin, levothyroxine, tacrolimus, cyclosporine, or any chemotherapy drug - be extra careful. These are the ones most likely to fail.
- Track your symptoms. If you start feeling worse after switching to a generic - even if it’s "the same drug" - don’t assume it’s your condition. Document everything: dates, symptoms, lab results.
- Ask for the brand. If you’ve had stability, and your doctor says you’re doing well - ask them to write "dispense as written" or "no substitution" on the prescription. It’s your right.
- Check for recalls. The FDA website has a searchable database. Sign up for alerts if you’re on a high-risk medication.
- Don’t accept a new generic without asking. If your pill looks different - color, shape, markings - ask the pharmacist why. And if they say "it’s the same," ask them to show you the manufacturer name. Write it down.
Some patients have had to go back to the brand-name drug - even if it costs $500 a month - just to survive. It’s not ideal. But it’s safer than gambling with a pill you can’t trust.

Why This Keeps Happening
The global generic drug market is worth $400 billion. That’s a lot of money. And a lot of pressure to cut costs.
Manufacturing in countries with weaker oversight is cheaper. But it’s also riskier. A factory in India might not have the same humidity controls as one in the U.S. A warehouse in Brazil might not have temperature monitoring. A shipment might sit in a port for weeks in 90-degree heat.
Regulators are overwhelmed. The FDA inspects only a fraction of foreign factories. And even when they find problems - like the nitrosamine contamination in blood pressure meds - they wait months to act. By then, millions of pills have been sold.
There’s no real system to track which batch went to which patient. No way to link a relapse in multiple sclerosis to a specific generic batch. No database that says: "This batch of tacrolimus from Company X in Mumbai has a 30% failure rate."
Until that changes, patients will keep getting sick - not because their disease is getting worse - but because the medicine they’re taking doesn’t work the way it should.
What Needs to Change
It’s not enough to say "generics are safe." That’s a blanket statement that’s killing people.
For high-risk drugs, bioequivalence standards need to be tighter - not 80-125%, but 90-111%, like they already are for some NTI drugs. Every batch needs to be tested, not just a few. Stability data needs to be public. Manufacturers need to be held accountable.
Patients need transparency. If you’re given a generic, you should know where it was made. When it was made. And whether it’s been recalled.
And doctors need to stop assuming generics are interchangeable. If a patient has been stable on a brand-name drug for years - don’t switch them unless you have to. And if they start failing - don’t assume it’s progression. Assume it’s the pill.
This isn’t about being anti-generic. It’s about being pro-safety. Millions of people take generics without issue. But for the ones who don’t - the ones who get sicker, or worse - the system failed them. And it’s still failing others right now.
Can a generic drug really be less effective than the brand name?
Yes. While most generics work fine, some have shown significant differences in how they release the active ingredient. For drugs with a narrow therapeutic index - like warfarin, phenytoin, or tacrolimus - even small changes in absorption can lead to treatment failure or toxicity. Cases have been documented where generic versions dissolved too quickly, degraded in storage, or contained inconsistent amounts of active ingredient - leading to relapses, organ damage, or death.
How do I know if my generic drug is safe?
Check the pill’s appearance and markings - if they’ve changed, ask your pharmacist why. Look up the manufacturer name and search the FDA’s recall database. If you’re on a high-risk medication (like an anticoagulant or transplant drug), monitor your symptoms and lab results closely after switching. If you notice sudden changes - fatigue, dizziness, seizures, or abnormal bleeding - contact your doctor immediately. You have the right to ask for the brand-name version if you’re concerned.
Why do pharmacies keep switching my generic medication?
Pharmacies are often required by insurance or Pharmacy Benefit Managers (PBMs) to choose the cheapest generic available. Even if you’ve been stable on one brand of generic, the pharmacy might switch you to another - cheaper - version without telling you. This is done to cut costs, not because it’s better for you. Always ask if a substitution was made, and request "dispense as written" on your prescription if you’re concerned.
What should I do if I think my generic drug isn’t working?
Don’t ignore it. Document your symptoms, when they started, and any changes in your medication. Contact your doctor right away - don’t wait for your next appointment. Ask if your drug could have changed manufacturers or if there’s been a recall. Request a blood test if applicable (like INR for warfarin). If your doctor dismisses your concerns, seek a second opinion. Your health is not something to gamble with.
Are all generic drugs risky?
No. The vast majority of generics are safe and effective. The problem is concentrated in a small subset of high-risk medications - those with a narrow therapeutic index - and in drugs manufactured under poor quality control. Antibiotics, statins, and many common prescriptions rarely have issues. But for transplant, cancer, heart, and seizure drugs, the stakes are much higher. Know which category your medication falls into, and be vigilant.
If you’re taking a high-risk generic drug, don’t assume it’s safe just because it’s cheap. Ask questions. Track your health. Demand transparency. Because when a generic doesn’t work - it’s not a glitch. It’s a warning.




Joseph Peel
November 18, 2025 at 20:21
There's a reason the FDA allows an 80-125% bioequivalence window for generics-it's statistically sound for most drugs. But you're absolutely right that for narrow therapeutic index medications, that margin is a liability. The system isn't broken because generics are bad-it's broken because we treat them all the same. We need tiered standards: stricter for anticoagulants, transplant meds, and seizure drugs. Period.
And yes, stability testing should be batch-specific, not random. If a pill degrades in transit from Mumbai to Miami, that’s not a manufacturing flaw-it’s a logistics failure. Someone needs to audit the supply chain, not just the pill itself.