Dispensing Errors: What They Are, Why They Happen, and How to Prevent Them
When a pharmacist hands you the wrong pill, the wrong dose, or a drug that clashes with your other meds, that’s a dispensing error, a preventable mistake in the final step of getting medicine to the patient. Also known as prescription errors, these aren’t just paperwork glitches—they’re a leading cause of preventable harm in healthcare. You might think pharmacies are foolproof, but the truth is, even the best systems break down under pressure. A 2023 study in the Journal of Patient Safety found that over 1.3 million dispensing errors occur each year in the U.S. alone—and nearly half of them reach the patient. Many go unreported because people don’t realize something’s wrong until it’s too late.
These errors don’t happen in a vacuum. They’re tied to medication safety, the system of practices designed to prevent harm from drugs. Poor labeling, rushed staff, similar-looking drug names, and outdated electronic systems all feed into the problem. For example, mixing up hydroxyzine and hydralazine sounds like a typo, but one treats anxiety, the other high blood pressure—and giving the wrong one can land you in the ER. Drug interactions, when two or more medications react dangerously are another big risk. Think St. John’s Wort messing with SSRIs, or antibiotics triggering C. diff. These aren’t theoretical. They show up in real patient stories, like the one in our posts where someone ended up with aplastic anemia after being given chloramphenicol without a proper allergy check.
What makes this worse is that many patients don’t know what to look for. You might assume your pharmacist double-checked everything. But if you don’t verify the name, dose, or color of the pill—especially when it’s a new prescription—you’re leaving safety to chance. Even small things matter: a 10 mg tablet instead of 5 mg, a liquid instead of a pill, or a different manufacturer’s version that doesn’t work the same. That’s why pharmacy mistakes, including mislabeling, wrong quantity, or incorrect directions are so dangerous. They’re silent until the side effects start.
There’s no magic fix, but you can cut your risk dramatically. Always check the label against your prescription. Ask: Is this what my doctor ordered? Does it match what I got last time? Is the dose right? Keep a written list of all your meds and allergies, and update it with every provider. If something feels off—like a pill that looks different or a new side effect you’ve never had—don’t ignore it. Talk to your pharmacist. They’re trained to catch these things, but they can’t if you don’t speak up.
Below, you’ll find real cases and clear guides on how these errors happen—and how to stop them before they hurt you. From nitrosamine contamination in generics to why authorized generics sometimes fail, these posts don’t just explain the problem. They give you the tools to protect yourself. Because when it comes to your meds, you’re not just a patient—you’re the last line of defense.
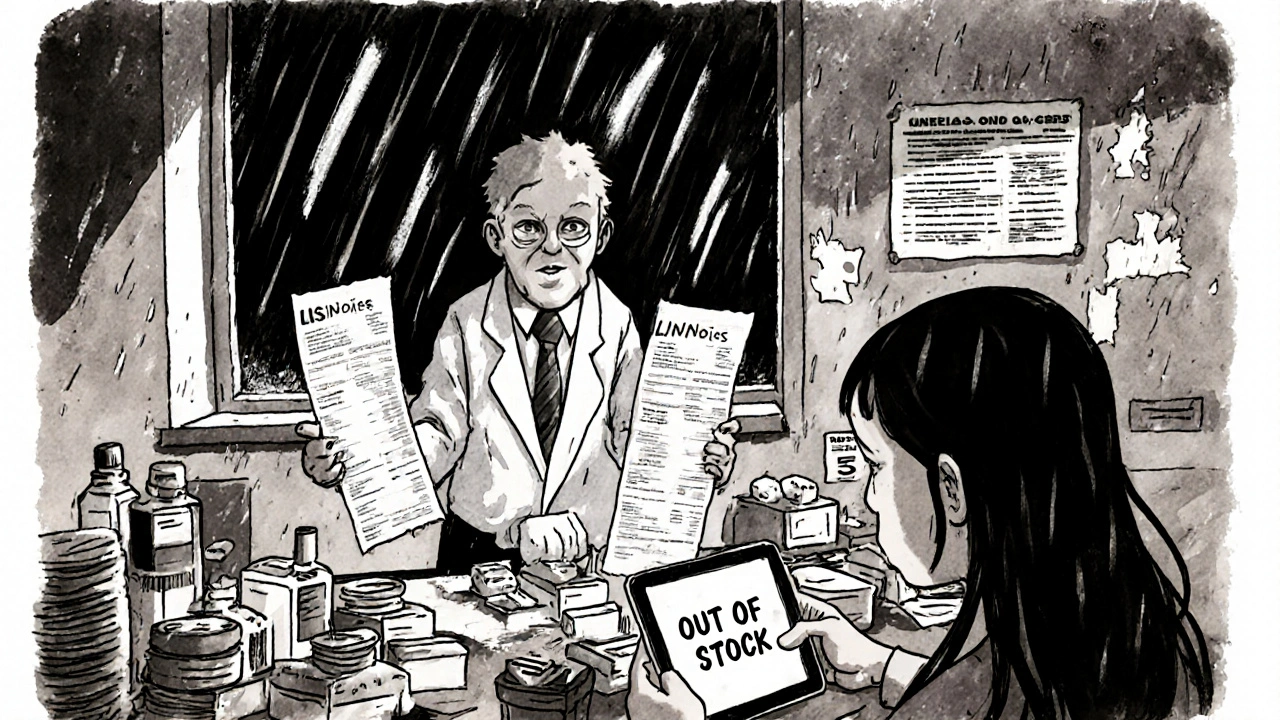
How to Handle Partial Fills and Back-Orders Without Errors in Pharmacy Operations
Learn how to manage partial fills and back-orders in pharmacies without risking dispensing errors. Real-world strategies for inventory tracking, billing, communication, and staff training to keep patients safe and satisfied.
About
Online Pharmacies
Latest Posts
Buy Cheap Generic Ciprofloxacin Online - Safe 2025 Guide
By Orion Kingsworth Oct 7, 2025
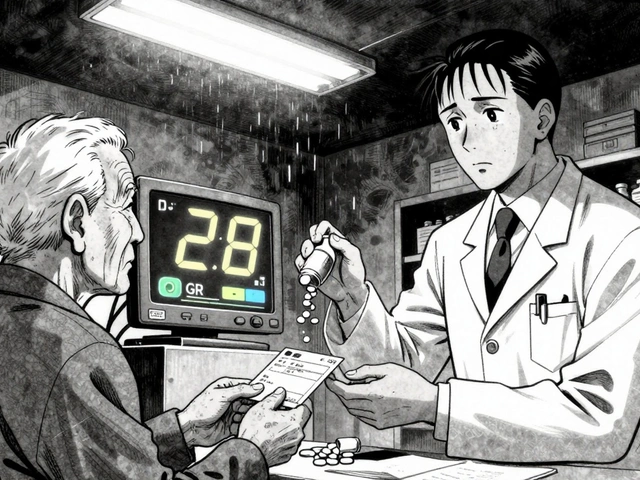
Medication Dosing Adjustments: How Age, Weight, and Kidney Function Change Your Prescription
By Orion Kingsworth Dec 12, 2025