Getting the right dose of medication isn’t just about following the label. For many people, the standard dose on the bottle could be too much-or too little-because of their age, weight, or how well their kidneys are working. Too high a dose can cause dangerous side effects. Too low a dose might mean the drug doesn’t work at all. This isn’t theoretical. In hospitals across the U.S., medication dosing errors tied to kidney function alone lead to thousands of preventable injuries every year.
Why One Size Doesn’t Fit All
Most drug labels give a single dose: "Take 500 mg twice daily." But that’s meant for a healthy adult, around 70 kg, with normal kidney function. It doesn’t account for the fact that older adults often have slower kidney clearance, or that someone who weighs 120 kg processes drugs differently than someone who weighs 45 kg. Even more, if your kidneys aren’t filtering blood properly, the drug can build up to toxic levels.Think of your kidneys like a filter in a coffee maker. If the filter is clogged, the coffee drips too slowly-or worse, overflows. The same thing happens with medications. Drugs like vancomycin, metformin, and certain antibiotics are cleared almost entirely by the kidneys. If those filters are worn out, the drug lingers. That’s why a 75-year-old with Stage 3 kidney disease might need half the dose of a 35-year-old with perfect kidneys-even if they have the same diagnosis.
How Kidney Function Changes Everything
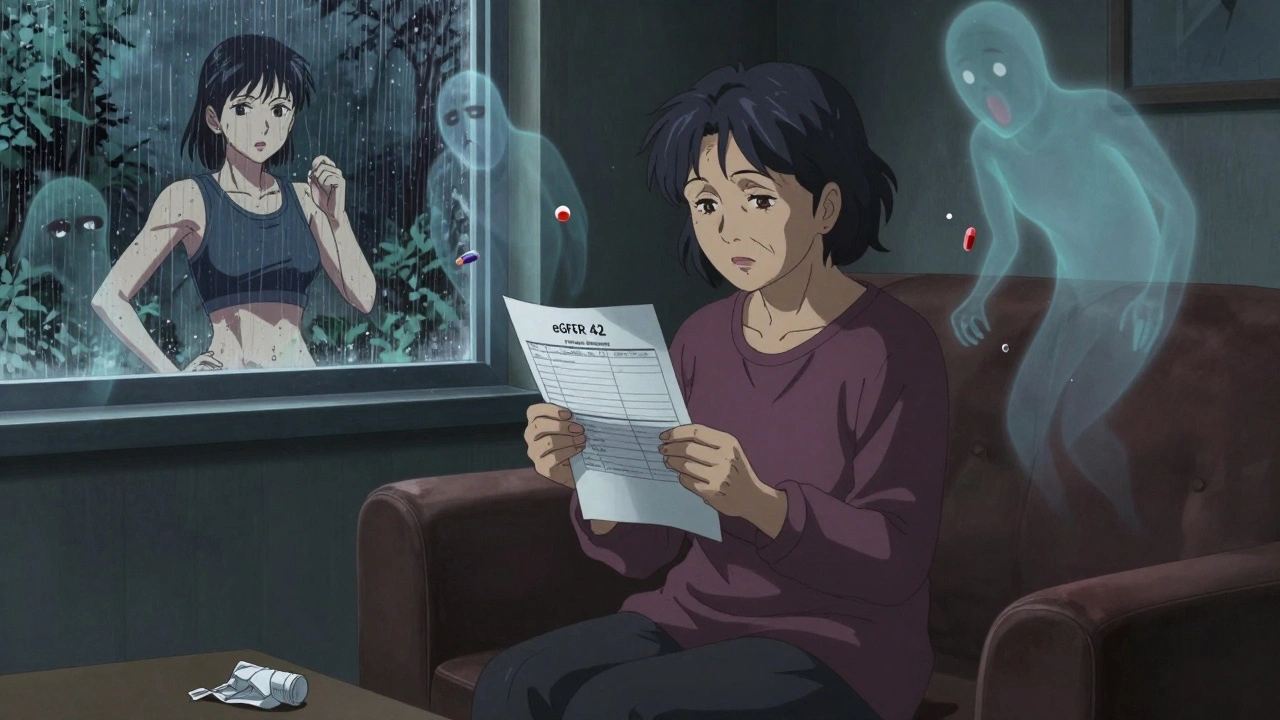
Doctors don’t just guess how well your kidneys are working. They use lab tests to estimate your glomerular filtration rate, or eGFR. This number tells them how efficiently your kidneys filter waste. The standard test is a blood draw for creatinine, then plugged into a formula.There are two main formulas in use today. The CKD-EPI equation is the current gold standard for diagnosing chronic kidney disease. It’s more accurate for most people, especially those with normal or near-normal kidney function. But here’s the catch: for dosing medications, doctors still often rely on the Cockcroft-Gault equation. Why? Because most drug guidelines were built using that older formula. It estimates creatinine clearance (CrCl) in mL/min, which directly matches how drug manufacturers tested dosing in clinical trials.
Here’s how they break it down:
- eGFR ≥ 90: Normal kidney function. Standard dose usually fine.
- eGFR 60-89: Mild reduction. Most drugs don’t need adjustment.
- eGFR 30-59: Moderate reduction (Stage 3). Many drugs need dose lowered or given less often.
- eGFR 15-29: Severe reduction (Stage 4). Strongly limit or avoid renally cleared drugs.
- eGFR < 15: Kidney failure (Stage 5). Often requires dialysis and major dose changes.
For example, metformin-a common diabetes drug-is officially contraindicated if eGFR falls below 30. Yet, many patients are still prescribed it at higher doses. One pharmacist in Chicago reported catching a patient on 1,000 mg twice daily with an eGFR of 28. That’s a serious risk for lactic acidosis. The correct max dose? 500 mg once daily.
Weight Matters More Than You Think
Weight isn’t just about body mass. It’s about how much space the drug has to spread through your body and how your liver and kidneys handle it. For people with obesity (BMI over 30), using actual body weight in dosing calculations can lead to overdosing. Why? Because fat tissue doesn’t help clear drugs-it just adds bulk.That’s why pharmacists use adjusted ideal body weight for dosing in obese patients. Here’s how it works:
- Calculate ideal body weight (IBW): For men, 50 kg + 2.3 kg for every inch over 5 feet. For women, 45.5 kg + 2.3 kg per inch over 5 feet.
- Then use: Adjusted weight = IBW + 0.4 × (actual weight − IBW)
For example, a 6-foot-tall man weighing 110 kg has an IBW of about 78 kg. His adjusted weight is 78 + 0.4 × (110 − 78) = 90.8 kg. Using 110 kg for dosing could mean giving him 25% more drug than needed. That’s dangerous with drugs like heparin or vancomycin, where even small overdoses can cause bleeding or hearing loss.
On the flip side, underweight patients (BMI under 18.5) often have lower muscle mass and reduced creatinine production. This makes eGFR calculations inaccurate. The Cockcroft-Gault equation overestimates their kidney function by up to 25%. That means they might get a dose meant for a healthy person, when they actually need less. A 55-year-old woman weighing 42 kg with normal creatinine might look fine on paper-but her real kidney clearance could be half what the formula says.
Aging Changes How Your Body Handles Drugs
As you get older, your kidneys naturally lose function. Even if your creatinine looks normal, your eGFR may be dropping. That’s why nearly 40% of adults over 65 have Stage 3 or worse kidney disease-without knowing it.But it’s not just kidneys. Older adults have less total body water, more body fat, and slower liver metabolism. This changes how drugs are absorbed, distributed, and broken down. Drugs like benzodiazepines, antipsychotics, and digoxin can build up and cause dizziness, falls, confusion, or heart rhythm problems.
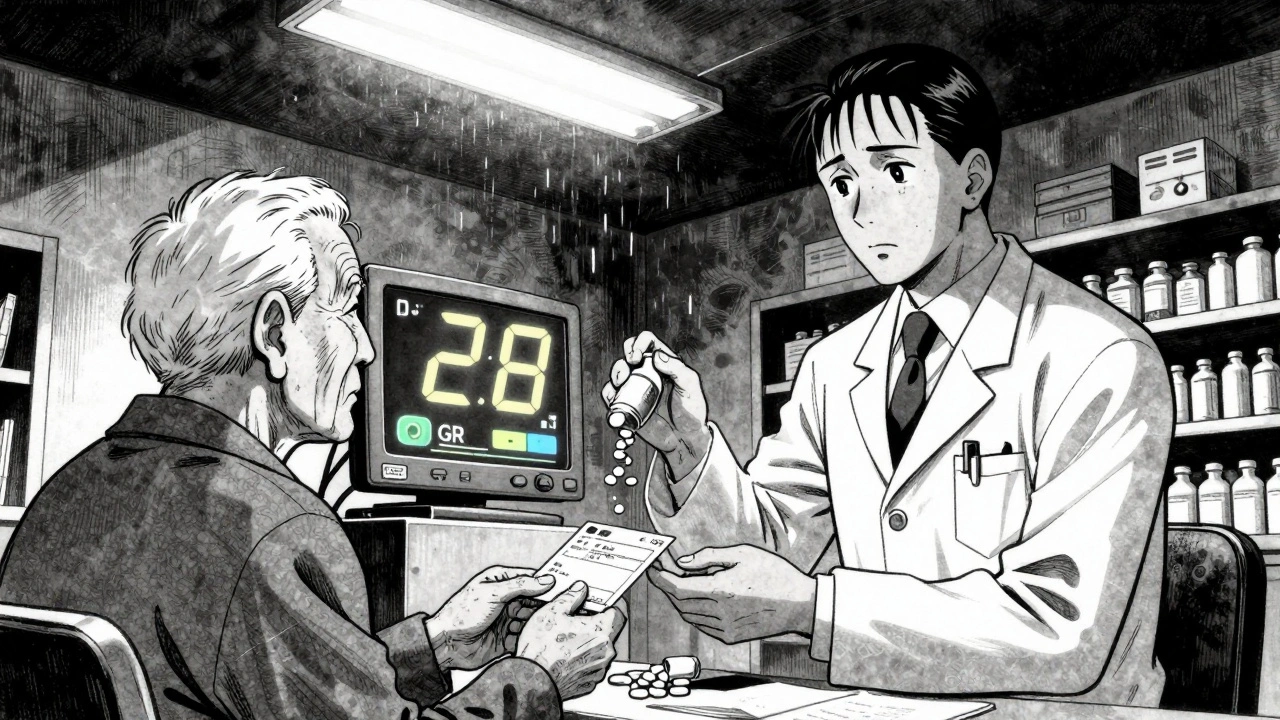
Studies show that 30% of adverse drug events in older adults are due to inappropriate dosing in kidney impairment. Yet, many doctors still default to standard doses because they don’t have time to calculate or don’t know the right formula. A 2022 survey found that emergency room doctors get renal dosing right less than 60% of the time.
That’s why automated alerts in electronic health records are a game-changer. One hospital system reduced dosing errors by 47% just by adding real-time CrCl calculations that flagged high-risk prescriptions before they were dispensed. Still, not every system uses the right formula. Some still use eGFR for dosing, which can be misleading in obese or elderly patients.
What You Can Do
You don’t need to be a doctor to protect yourself. Here’s how to stay safe:- Ask your pharmacist: "Is this dose right for my kidney function?" They can pull your latest eGFR or CrCl from your chart.
- Know your numbers. If you’ve had a blood test for creatinine in the last 6 months, ask for your eGFR result. Write it down.
- Don’t assume a new prescription is safe. If you’re over 65, overweight, or have diabetes or high blood pressure, assume your kidneys aren’t working at 100% until proven otherwise.
- Use apps or tools. Many pharmacy apps now show renal dosing warnings. If yours doesn’t, ask for a printed dosing guide from your pharmacist.
- Speak up if you feel dizzy, confused, or nauseous after starting a new drug. It might not be a side effect-it might be an overdose.
The Bigger Picture: Why This Is Still a Problem
Even with all the science, inconsistencies remain. One hospital might say to reduce cefazolin by 50% at eGFR 20-29. Another says 75%. A third says no adjustment needed. A 2023 study found 38% of antibiotic dosing guidelines for kidney patients contradict each other across major references.Pharmacists spend 5 to 7 minutes per patient just checking renal dosing. That’s time they don’t have in busy clinics. And while AI-driven dosing tools are coming-some using genetic data and wearable sensors to predict kidney function in real time-most clinics still rely on outdated formulas and paper charts.
The cost of getting it wrong is high. The Medicare program estimates that improper renal dosing adds $3.2 billion a year in avoidable hospitalizations. But beyond the money, it’s about safety. A single wrong dose can send an elderly person to the ER-or worse.
Final Thought: It’s Not Just a Number
Your dose isn’t just a number on a prescription. It’s a calculation shaped by your body, your age, your weight, and how your kidneys are doing today. No two people are the same. And no two doses should be either.Ask questions. Know your numbers. Don’t let a generic label be the only guide. Your body is unique. Your medication should be too.
How do I know if my medication dose needs adjusting for kidney function?
Your doctor or pharmacist should check your estimated glomerular filtration rate (eGFR) or creatinine clearance (CrCl) from a recent blood test. If your eGFR is below 60 mL/min/1.73m², or if you’re over 65, overweight, or have diabetes or high blood pressure, ask whether your dose needs adjustment. Many common drugs-like metformin, antibiotics, and painkillers-require changes at this level.
Is eGFR or CrCl better for dosing medications?
For diagnosing kidney disease, eGFR (using the CKD-EPI formula) is the standard. But for dosing medications, CrCl (calculated with the Cockcroft-Gault equation) is still preferred. That’s because most drug labels were tested and approved using CrCl. Using eGFR alone for dosing can lead to overdosing, especially in obese or elderly patients.
Should I use my actual weight or ideal weight for dosing calculations?
If you’re obese (BMI over 30), use adjusted ideal body weight-not your actual weight. This prevents overdosing. For underweight people (BMI under 18.5), actual weight may be more accurate because low muscle mass can make creatinine levels misleading. Always ask your pharmacist which weight to use for your specific drug.
What drugs are most likely to need kidney adjustments?
Antibiotics like vancomycin and cefazolin, diabetes drugs like metformin and SGLT2 inhibitors, pain relievers like morphine and gabapentin, heart medications like digoxin and furosemide, and seizure drugs like phenytoin all commonly require dose changes with kidney impairment. Always check the label or ask your pharmacist.
Can I just take half the dose if I’m older or have kidney disease?
No. Some drugs need reduced doses, others need longer gaps between doses, and some should be avoided entirely. Halving a dose without knowing the drug’s pharmacokinetics can make it ineffective or dangerous. Always follow a professional’s guidance based on your specific lab results and drug profile.




Cole Newman
December 13, 2025 at 03:44
Bro, I saw this guy on TikTok say his grandma died because the hospital gave her the wrong dose of vancomycin and they didn't check her CrCl. Like, how is this still a thing in 2025? I work in IT and even my dumb hospital app has a pop-up that says "CRCL BELOW 30, DOSE REDUCED". Why are doctors still eyeballing this? It's not rocket science.