MAO-B Inhibitor: What It Is, How It Works, and What You Need to Know
When you hear MAO-B inhibitor, a type of drug that blocks the enzyme monoamine oxidase B to increase dopamine levels in the brain. Also known as dopamine-preserving agent, it's not a cure—but for people with Parkinson’s, it can mean more movement, fewer tremors, and better days. Unlike older antidepressants that hit multiple brain chemicals, MAO-B inhibitors are focused. They don’t mess with serotonin or norepinephrine much. They target just one enzyme—MAO-B—that breaks down dopamine. Less breakdown means more dopamine available where it’s needed: in the parts of the brain that control movement.
This makes them a key tool in Parkinson’s disease, a progressive neurological disorder caused by loss of dopamine-producing cells treatment. They’re often used early on, sometimes alone, sometimes with levodopa. Two names you’ll see most often are selegiline, a once-daily pill that can delay the need for stronger meds and rasagiline, a similar drug with fewer dietary restrictions and a cleaner side effect profile. Both are taken orally, both are long-term, and both are designed to help people stay active longer. They don’t stop the disease, but they slow down the symptoms that make daily life harder—like stiffness, slow movements, and freezing episodes.
What’s interesting is how these drugs fit into bigger patterns you’ll see in the posts below. You’ll find posts about MAO-B inhibitor use alongside discussions on drug interactions, genetic differences in how people respond to meds, and even how to manage side effects without ditching the benefits. Some people on these drugs also take statins or blood pressure meds—so you’ll see overlap with posts about SLCO1B1 gene testing or Valsartan-Hydrochlorothiazide and potassium levels. Others are managing multiple conditions, like acromegaly or atrophic gastritis, which can affect how drugs are absorbed or metabolized. That’s why knowing how MAO-B inhibitors behave in the body matters—not just for Parkinson’s, but for anyone on more than one long-term medication.
You won’t find a post here that says "take this and feel better." But you will find real, practical comparisons—what works, what doesn’t, what to watch out for, and how to make it last. Whether you’re a patient, a caregiver, or just trying to understand why your doctor chose this drug over another, the posts below give you the details without the fluff. No hype. Just what you need to know to make sense of your treatment.
Rasagiline’s Role in Slowing Parkinson’s Disease Progression
Explore how rasagiline works, its neuroprotective evidence, and practical tips for using it to potentially slow Parkinson's disease progression.
About
Medications
Latest Posts


Behavioral Economics: Why Patients Choose Certain Drugs Over Others
By Orion Kingsworth Dec 8, 2025
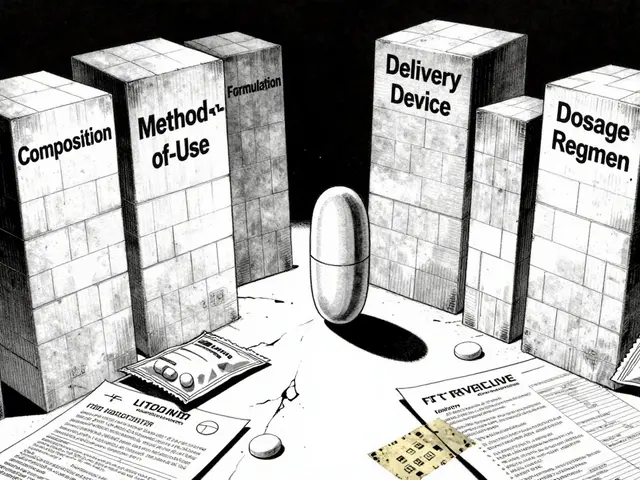
Formulation Patents on Drug Combinations: How Brands Extend Exclusivity
By Orion Kingsworth Feb 11, 2026

Benzodiazepines and Birth Defect Risks: What Pregnant Women Need to Know
By Orion Kingsworth Feb 7, 2026