NDMA: What It Is, Why It Matters in Medications, and How to Stay Safe
When you take a pill, you expect it to help—not hurt. But some medications have been found to contain NDMA, a probable human carcinogen that forms during certain chemical processes and can contaminate drugs during manufacturing. Also known as N-nitrosodimethylamine, it’s not added on purpose—it sneaks in as an impurity, often in drugs made with specific chemical reactions or under poor quality controls. This isn’t theoretical. Back in 2018, the FDA started pulling valsartan, losartan, and other blood pressure meds off shelves after NDMA turned up in batches made by certain overseas factories. Since then, metformin, ranitidine, and even some Zantac versions were recalled for the same reason.
NDMA doesn’t show up in every pill. But when it does, the risk isn’t just about one bad batch—it’s about long-term exposure. The FDA says even small amounts, taken daily over years, could raise cancer risk. That’s why they set strict limits: no more than 96 nanograms per day. Some contaminated pills had hundreds of times that. The real problem? Nitrosamines, a family of chemical compounds that includes NDMA and can form when amines react with nitrites under heat or acidic conditions. These aren’t just in meds—they’re in cured meats, tobacco smoke, and even some water supplies. But in pharmaceuticals, it’s the manufacturing process that’s the main culprit: outdated equipment, uncontrolled reactions, or low-grade raw materials from suppliers with weak testing. That’s why China’s generic drug factories have been under heavy FDA scrutiny—over 70% of active ingredients come from there, and inspection reports show repeated failures in contamination controls.
You won’t know if your medicine has NDMA just by looking at it. The FDA doesn’t test every pill in every bottle. Instead, they issue recalls based on lab findings and manufacturer reports. If your drug was pulled, you’ll hear about it from your pharmacy or the FDA website. But here’s the thing: if you’re on a medication that’s been recalled before—like blood pressure pills or diabetes drugs—it’s smart to ask your doctor or pharmacist if your current batch is safe. Switching to a different brand or generic version can help. And if you’ve been taking a recalled drug for months or years, talk to your doctor about whether you need screening for liver or stomach cancer. It’s not panic—it’s prevention.
What’s below is a collection of real-world stories and facts about drug safety, contamination, and how generics can go wrong. You’ll find posts on FDA alerts, Chinese manufacturing risks, why some generics fail, and how to spot when your medicine isn’t what it claims to be. None of this is guesswork. It’s all based on inspections, recalls, and patient reports. You’re not alone in wondering if your meds are safe. These posts will help you find out—and what to do next.
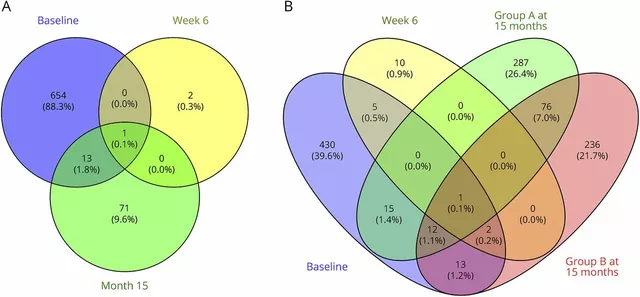
Nitrosamine Contamination in Generic Drugs: Recent Recalls and Regulatory Shifts
Nitrosamine contamination in generic drugs has led to over 500 FDA recalls since 2018. Learn which medications were affected, why it happened, how regulators responded, and what it means for your health.
About
Medications
Latest Posts

How to Buy Cheap Generic Tamoxifen Online Safely
By Orion Kingsworth Oct 4, 2025

How Environmental Factors Influence Bronchial Asthma
By Orion Kingsworth Oct 1, 2025
Dimethyl Fumarate: A Game Changer in Treating Autoimmune Diseases
By Orion Kingsworth Apr 29, 2023