When you’re a veteran relying on VA healthcare, your prescription drugs aren’t just covered-they’re carefully managed. The VA formulary isn’t a simple list of approved meds. It’s a tightly controlled system built to give you the right drugs at the lowest possible cost, with generics as the default. If a generic version exists, that’s what you’ll get-unless your provider can prove you need the brand name for medical reasons.
How the VA Formulary Works
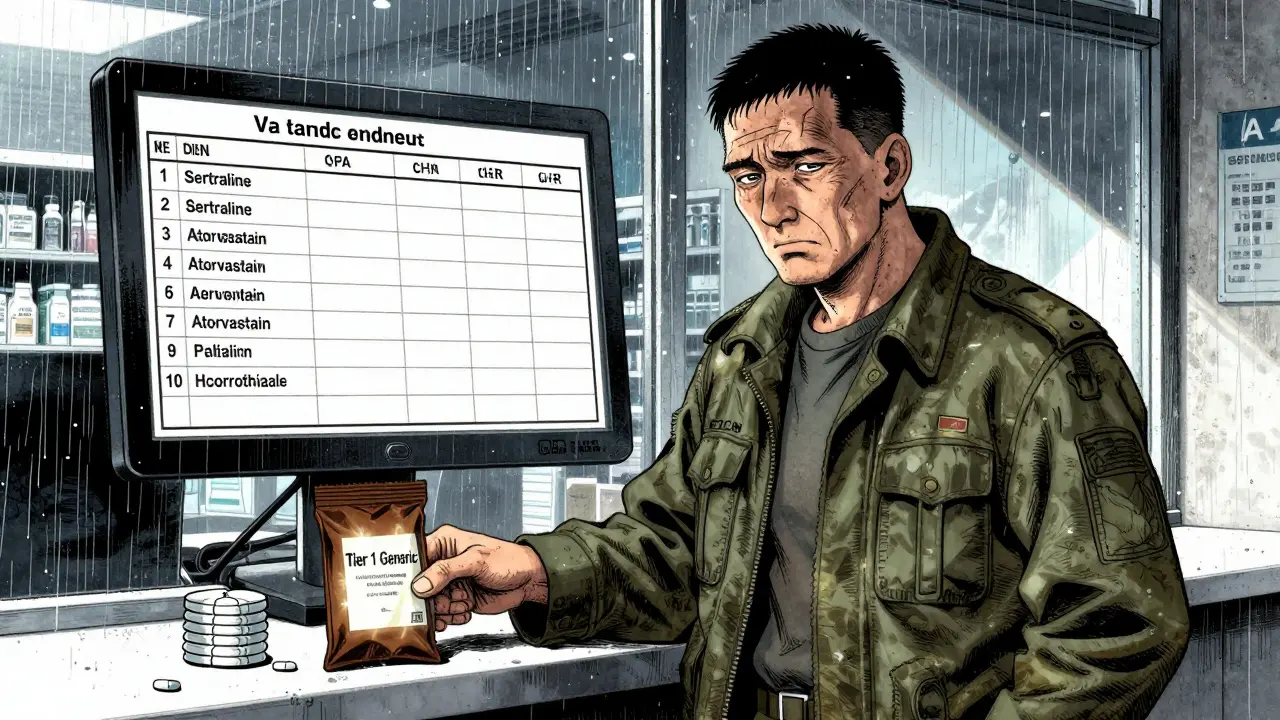
The VA National Formulary is the single, mandatory list of all medications available at every VA facility across the country. It’s updated every month, with changes published in official newsletters. Unlike commercial insurers that might have five or six tiers, the VA uses just three. Tier 1 is for preferred generics. Tier 2 is for non-preferred generics or lower-cost brands. Tier 3 is for higher-cost brand-name drugs or specialty medications.
Here’s the key: if a generic version of your drug is available, the VA will cover only the generic. That’s not a suggestion-it’s policy. This rule applies to everything from blood pressure pills to antidepressants. For example, if you’re on sertraline, you’ll get the generic version, not Zoloft. The same goes for atorvastatin instead of Lipitor, or hydrochlorothiazide instead of Microzide.
This system saves veterans money. A 30-day supply of a Tier 1 generic typically costs $5 to $10. Compare that to commercial insurance, where the same drug might cost $20 to $50 out of pocket. The VA’s generic-first approach drives a 92% usage rate of generics-higher than any other major U.S. payer, including Medicare Part D.
Tier 1 Drugs: What’s Covered for Free or Low Cost
Tier 1 is where most veterans stay. These are the most cost-effective, clinically proven generics. As of 2025, here are some common Tier 1 medications:
- Alendronate (for osteoporosis)
- Aspirin buffered tablets (for heart health)
- Allopurinol (for gout)
- Ibuprofen (for pain and inflammation)
- Atorvastatin (for high cholesterol)
- Ezetimibe (cholesterol combo drug)
- Pravastatin (another statin option)
- Furosemide (for fluid retention)
- Hydrochlorothiazide (blood pressure)
- Fluoxetine (for depression and anxiety)
- Sertraline HCL (another antidepressant)
- Trazodone (for sleep and depression)
These drugs aren’t randomly chosen. They’re selected based on clinical effectiveness, safety, and cost. The VA’s National Drug Formulary Committee reviews new drugs monthly using real-world data, not marketing claims. If a generic version of a drug is proven to work just as well-and costs less-it gets added to Tier 1.
Why Generics Are the Rule, Not the Exception
You might wonder: are generics really the same? The answer is yes-when it comes to active ingredients, absorption, and effectiveness. The FDA requires generics to meet the same strict standards as brand names. The VA doesn’t take this on faith-it tracks outcomes. Studies show no difference in hospitalizations, side effects, or treatment success between brand and generic versions of the same drug.
Some veterans worry at first. A 2024 VA survey found that 12% of users had initial concerns about generic effectiveness. But after talking with their provider and seeing results, 94% continued taking the generic without issue. Real-world stories back this up. One veteran on Reddit wrote: “Switched to generic sertraline through VA Mail Order-same effect as Zoloft, but $0 copay instead of $15 at my local pharmacy.”
The VA’s savings are massive. In 2024 alone, the formulary system saved $2.8 billion in pharmaceutical costs. That’s money that stays in the system to help more veterans.
What’s Not Covered-And How to Get It
Not every drug is on the formulary. Newer specialty drugs, especially for weight loss or rare conditions, often face restrictions. For example, GLP-1 medications like Wegovy, Ozempic, and Mounjaro are covered-but only for FDA-approved uses. That means Wegovy is covered for weight loss only if you have cardiovascular disease or obesity with related conditions. It’s not covered for general weight loss.
If your provider wants a drug that’s not on the formulary, you’ll need prior authorization. This isn’t a red tape trap-it’s a safety check. The VA reviews each request based on clinical need, alternatives available, and cost-effectiveness. Some veterans report long waits, especially for newer drugs. One user on the Veterans Benefits Network wrote: “My doctor wanted me on Wegovy for weight, but the VA only covers it for diabetes. Had to appeal for three months.”
CHAMPVA beneficiaries (spouses and dependents of veterans) follow the same rules. As of January 2025, they can get GLP-1 drugs only for type 2 diabetes, obstructive sleep apnea, or cardiovascular disease-not for cosmetic weight loss.
How to Use the System: VA Pharmacy, Meds by Mail, and Community Care
You have three ways to get your prescriptions:
- VA Pharmacy: Pick up at any VA clinic or hospital. Bring your VA ID and prescription.
- Meds by Mail: Order maintenance medications (like blood pressure or diabetes drugs) to be delivered to your home. No copay, no deductible for CHAMPVA users. This is the most popular option-87% of users rate it positively.
- Community Care: If you’re far from a VA facility, you can use a local pharmacy under the VA’s Community Care program. But here’s the catch: the pharmacy must follow the VA formulary. If they don’t have the generic, they can’t bill the VA.
The VA Formulary Advisor tool on VA.gov lets you search any drug by name and see its tier, copay, and whether it’s covered. You can also download the full list in Excel or CSV format. It’s updated monthly.

Common Problems and How to Fix Them
Even with a strong system, issues come up:
- Confusing tiers: 35% of new enrollees don’t understand why some drugs cost more. Check the formulary tool before filling a prescription.
- Out-of-pocket surprises: If a pharmacy tries to charge you more than the VA copay, show them your VA benefits card. The VA sets the price.
- Delayed authorizations: For non-formulary drugs, start the prior authorization process early. Have your provider submit clinical notes that explain why the generic won’t work.
- Medication switches: If your doctor changes your drug, ask if there’s a generic version on Tier 1. Don’t assume the brand is better.
VA pharmacy staff are trained to help. Call the VA Pharmacy Benefits line at 1-800-877-8339. They handle 18,000 calls a day and can walk you through coverage, prior auth, or mail-order setup.
What’s Changing in 2026
The VA is making the system even smarter. By late 2026, AI tools will be built into electronic health records to suggest generic alternatives in real time when a provider writes a prescription. This will reduce delays and improve adherence.
The VA is also expanding coverage for oncology and rare disease drugs, though cost controls will remain tight. A 2025 Congressional Budget Office report found the current system is financially sustainable through 2030-but recommends investing in pharmacogenomic testing. That means testing your genes to predict which drugs work best for you, reducing trial-and-error prescribing.
For now, the system works. Veterans pay less, get the same results, and have access to over 9 million people nationwide. The VA’s formulary isn’t perfect, but it’s one of the most efficient, evidence-based, and veteran-focused pharmacy systems in the country.
Are all VA prescriptions generic?
No, but generics are the default. If a generic version of your medication exists and is approved by the FDA, the VA will cover only the generic unless your provider documents a medical reason why you need the brand name. This is standard policy across all VA facilities.
How do I check if my drug is covered by the VA?
Use the VA Formulary Advisor tool on VA.gov. Search by drug name, and it will show you the tier, copay amount, and whether it’s covered. You can also download the full monthly formulary list in Excel or CSV format.
Can I get brand-name drugs through the VA?
Only if there’s no generic available, or if your provider submits a prior authorization request explaining why the generic won’t work for you. Common reasons include severe allergies to inactive ingredients or documented lack of effectiveness with the generic version.
Does the VA cover weight loss drugs like Wegovy?
Yes-but only for specific FDA-approved uses. As of January 2025, Wegovy is covered only for adults with obesity and cardiovascular disease, or for metabolic-associated steatohepatitis. It’s not covered for general weight loss. Other GLP-1 drugs like Ozempic and Mounjaro are covered only for type 2 diabetes.
What’s the difference between VA and Medicare Part D formularies?
VA has only three tiers with lower copays and a strict generic-first policy. Medicare Part D typically has five tiers with higher out-of-pocket costs and less consistent generic coverage. For example, a drug like atorvastatin might cost $5 at the VA but $35 or more on a Medicare plan with a high deductible.
How do I get my prescriptions delivered to my home?
Sign up for Meds by Mail through VA.gov. You’ll need to enroll, then your provider can send prescriptions electronically. Maintenance medications like blood pressure or diabetes drugs are shipped in 90-day supplies with no copay for most veterans. Refrigerated drugs like biologics may have shipping restrictions.




Sarah Mailloux
January 14, 2026 at 18:50
Just got my 90-day supply of sertraline through Meds by Mail-$0 copay, shipped to my door. No more driving 45 minutes to the VA clinic. This system works.