When you're pregnant and struggling with severe anxiety or insomnia, the pressure to find relief is real. But if you're taking benzodiazepines-medications like Xanax, Valium, or Lorazepam-you need to understand the risks. These drugs don’t just affect you. They cross the placenta. And they can affect your baby’s development.
What Are Benzodiazepines, and Why Are They Used During Pregnancy?
Benzodiazepines are a class of drugs developed in the 1950s to calm the nervous system. They work by boosting GABA, a brain chemical that reduces anxiety and promotes sleep. For many women, they’re a lifeline-especially those with treatment-resistant anxiety or panic disorders.
But here’s the catch: even when taken as prescribed, benzodiazepines easily pass through the placenta. By the time they reach the fetus, they’re still active. And during the first trimester-when organs are forming-that’s when the risk is highest.
Studies show about 1.7% of pregnant women in the U.S. get a benzodiazepine prescription in the first trimester. That number is rising. Why? Because anxiety and sleep disorders affect roughly 1 in 6 women of childbearing age. Many don’t realize these drugs carry risks, or they’re told by a provider that the benefits outweigh the dangers.
What Birth Defects Are Linked to Benzodiazepines?
The evidence isn’t simple. Some studies say the risk is small. Others point to serious, rare defects. Let’s break it down.
A 2022 study of over 3 million pregnancies in South Korea found that first-trimester benzodiazepine use was tied to a slightly higher risk of overall birth defects-about 8 extra cases per 1,000 exposed pregnancies. The biggest concern? Heart defects. For every 1,000 women exposed, about 14 more babies had heart problems compared to unexposed pregnancies.
But some defects are rarer-and more alarming. The CDC’s National Birth Defects Prevention Study, which looked at over 11,000 pregnancies, found strong links between specific benzodiazepines and rare conditions:
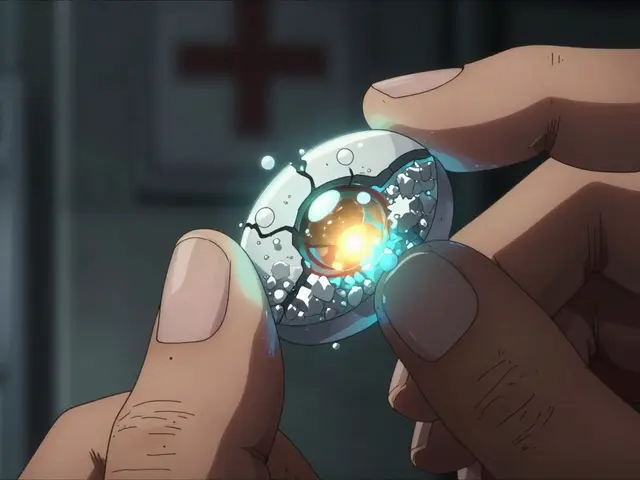
- Dandy-Walker malformation (a brain development issue): 3 times higher risk
- Anophthalmia or microphthalmia (missing or underdeveloped eyes): 4 times higher risk, especially with alprazolam
- Esophageal atresia (a blocked or disconnected food tube): 2.7 times higher risk with alprazolam
- Pulmonary valve stenosis (a narrowed heart valve): 4 times higher risk with lorazepam
These are rare outcomes. But when they happen, they’re life-changing. And the pattern isn’t random. The risk jumps with higher doses. If you’re taking more than 2.5 mg of lorazepam-equivalent daily, your risk goes up even more.
Why Do Some Studies Say There’s No Risk?
You might have heard that benzodiazepines are safe during pregnancy. That’s because some studies didn’t find a link. A 2023 study in the British Journal of Clinical Pharmacology reported no significant increase in birth defects. So which one do you believe?
The difference? Confounding by indication. That’s a fancy way of saying: maybe it’s not the drug causing the problem-it’s the condition the drug treats. If a woman has severe anxiety, her stress levels, sleep habits, or even smoking or alcohol use might be higher. Those factors can also cause birth defects.
But here’s the key: the 2022 PLOS Medicine study didn’t just look at the data. They ran negative control analyses. That means they tested whether the same pattern showed up with unrelated conditions-like a broken bone or a cold. It didn’t. That’s strong evidence the link is real, not just a side effect of the underlying illness.
And when you combine all the data, the weight of evidence is shifting. The 2022 study had 10 times more exposed pregnancies than all previous studies combined. That’s not a fluke. That’s science.
Other Risks Beyond Birth Defects
Benzodiazepines aren’t just a risk for physical defects. They affect the whole pregnancy.
- Miscarriage: A 2024 JAMA Psychiatry study found an 85% higher risk of miscarriage among women who used benzodiazepines during pregnancy.
- Preterm birth: Babies born early are more likely to need NICU care, have breathing problems, or face long-term developmental delays.
- Low birth weight and small size: These babies struggle to regulate temperature, feed properly, and fight infections.
- Low Apgar scores: This measures how well a newborn is adjusting after birth. Lower scores mean the baby needs more help.
- Ectopic pregnancy: Even exposure in the 90 days before conception was linked to a higher chance of this dangerous condition.
The absolute risk of each of these outcomes is still low. But when you stack them together-miscarriage, preterm birth, heart defects, brain malformations-the picture changes. It’s not just one risk. It’s a chain of risks.
What About Alprazolam? Is It Worse?
Yes. Alprazolam (Xanax) stands out.
Multiple studies point to alprazolam as the biggest concern for specific defects. It’s not just a general benzodiazepine risk-it’s a specific risk. Women who took alprazolam during pregnancy had:
- 4 times the risk of missing or underdeveloped eyes
- 2.7 times the risk of esophageal atresia
Why? We don’t fully know. Maybe it’s how the body breaks it down. Maybe it crosses the placenta more easily. Or maybe it affects fetal brain development in a unique way. Whatever the reason, the data is consistent. If you’re on alprazolam and pregnant-or planning to be-this isn’t a minor detail. It’s critical.
What Do Experts Say?
Guidelines are clear: avoid benzodiazepines in the first trimester if you can.
- ACOG (American College of Obstetricians and Gynecologists): Says benzodiazepines "may be used cautiously for short-term treatment" but should be avoided in the first trimester.
- U.S. FDA: Classifies them as Category D-"positive evidence of human fetal risk."
- European Medicines Agency: Recommends avoiding them in the first trimester unless absolutely necessary.
- Canadian Guidelines: Say they should "generally be avoided," but acknowledge exceptions for severe, treatment-resistant cases.
Even the American Psychiatric Association says: "Consider risks and benefits on a case-by-case basis." That’s not a green light. It’s a warning.
And here’s what they all agree on: Non-drug treatments should come first.

What Are the Alternatives?
You don’t have to suffer. There are safer ways to manage anxiety and sleep during pregnancy.
- Cognitive Behavioral Therapy (CBT): Proven to work as well as medication for anxiety. No drugs. No risk.
- Mindfulness and meditation: Studies show they reduce cortisol, lower anxiety, and improve sleep quality.
- Exercise: Even 30 minutes of walking most days helps regulate mood and sleep.
- Light therapy and sleep hygiene: For insomnia, avoiding screens before bed, keeping a consistent schedule, and using dim lighting can be more effective than sleeping pills.
- SSRIs (like sertraline): While not risk-free, they’re generally considered safer than benzodiazepines during pregnancy. Talk to your doctor about switching.
Many women stop benzodiazepines cold turkey-and that’s dangerous. Withdrawal can trigger seizures, panic attacks, or even harm the pregnancy. If you’re thinking of stopping, talk to your OB-GYN and a psychiatrist together. They can help you taper safely.
What Should You Do Right Now?
If you’re pregnant and taking benzodiazepines:
- Don’t panic. The absolute risk of major defects is still low.
- Don’t stop suddenly. Withdrawal can be dangerous.
- Do schedule an appointment. Bring your prescription list. Ask: "Is this still necessary?" "Are there safer options?" "Can we lower the dose?"
- Ask about timing. If you’re past the first trimester, the risk of birth defects drops. But other risks-like preterm birth or low Apgar scores-still exist.
- Track your dose. Keep a log: what you take, how much, and when. This helps your provider make smarter decisions.
If you’re trying to get pregnant:
- Start talking to your doctor before conception.
- Explore non-drug treatments now.
- If you’re on alprazolam, ask if switching to a different medication is possible.
What’s Next?
Researchers are working on better answers. The International Pregnancy Safety Study Consortium is tracking 5,000 pregnant women taking benzodiazepines from 2024 to 2026. They’re looking at specific drugs, doses, and timing. We’ll know more soon.
Until then, the message is clear: benzodiazepines aren’t harmless. They carry real, documented risks. But they’re not a death sentence. With careful planning, support, and alternatives, you can protect both your health and your baby’s.
Are benzodiazepines safe during pregnancy?
No, benzodiazepines are not considered safe during pregnancy, especially in the first trimester. Multiple large studies link them to increased risks of birth defects-including heart defects, brain malformations, and eye abnormalities-as well as miscarriage, preterm birth, and low birth weight. While the absolute risk for any individual is low, the evidence is strong enough that major medical groups recommend avoiding them unless absolutely necessary.
Is alprazolam (Xanax) more dangerous than other benzodiazepines during pregnancy?
Yes, alprazolam appears to carry higher risks for specific birth defects compared to other benzodiazepines. Studies have found a 4-fold increased risk of anophthalmia or microphthalmia (missing or underdeveloped eyes) and a 2.7-fold increased risk of esophageal atresia (a blocked food tube) in babies whose mothers took alprazolam during pregnancy. These associations were not seen with other benzodiazepines to the same degree, suggesting alprazolam may have unique effects on fetal development.
Can I stop taking benzodiazepines right away if I’m pregnant?
No. Stopping benzodiazepines suddenly can cause dangerous withdrawal symptoms, including seizures, severe anxiety, hallucinations, and even harm to the pregnancy. If you’re pregnant and taking these medications, work with your doctor and a psychiatrist to create a safe tapering plan. Never stop on your own.
What are the safest alternatives to benzodiazepines for anxiety during pregnancy?
Cognitive Behavioral Therapy (CBT) is the most effective non-drug treatment for anxiety during pregnancy. Other safe options include mindfulness practices, regular exercise, sleep hygiene, and light therapy. For medication, SSRIs like sertraline are generally considered safer than benzodiazepines and are often recommended when drug treatment is needed. Always consult your OB-GYN and mental health provider before making changes.
Should I avoid benzodiazepines if I’m trying to get pregnant?
Yes. Exposure to benzodiazepines in the 90 days before conception has been linked to an increased risk of ectopic pregnancy. Since the first trimester is the most critical time for fetal development, it’s best to switch to safer alternatives or stop the medication entirely before trying to conceive. Talk to your doctor at least 3-6 months before planning pregnancy to allow time for safe transitions.
There’s no easy answer when you’re pregnant and struggling. But you’re not alone. With the right support, you can find relief without putting your baby at risk.




Ashlyn Ellison
February 7, 2026 at 10:21
I took Xanax for like 3 weeks when I was 8 weeks pregnant. Didn’t tell anyone. My kid’s 4 now and perfectly healthy. Maybe I just got lucky.