Every time you visit a new doctor, pharmacist, or emergency room, your allergy list could be wrong. And if it is, you could be given a drug that triggers a life-threatening reaction-even if you’ve never had one before. This isn’t rare. In hospitals, 5% of patients suffer an adverse drug event because someone misread or missed an allergy note. That’s one in every 20 people. For penicillin allergies alone, inaccurate labels cost the U.S. healthcare system over $1.2 billion a year because doctors prescribe more expensive, less effective antibiotics out of caution.
You don’t need to be a medical professional to fix this. You’re the only person who truly knows your body. And with the right steps, you can make sure every provider you see has the correct, up-to-date version of your allergy list-even if they use different systems.
Why Your Allergy List Might Be Wrong
Many people think they’ve been told they’re allergic to something, but they never got tested. Maybe a rash appeared after taking amoxicillin as a kid. Or your mom said you were allergic to sulfa drugs. Maybe you had nausea after a painkiller and assumed it was an allergy. But nausea? That’s often a side effect, not an allergy. True allergies involve your immune system-hives, swelling, trouble breathing, anaphylaxis.
Doctors don’t always dig deep. In 2022, a study at Parkland Health found nearly 13% of recorded allergies were incorrect or outdated. One patient had a penicillin allergy listed since age 8. At 42, they’d taken it five times without issue. But the label stayed. Why? Because no one ever questioned it.
Even when systems talk to each other-like Epic and Cerner EHRs sharing data-they just copy and paste. They don’t check if the allergy is still valid. That’s called basic interoperability. It’s better than nothing, but it’s not enough. A 2022 AHRQ study showed 38% of cross-system allergy records had errors.
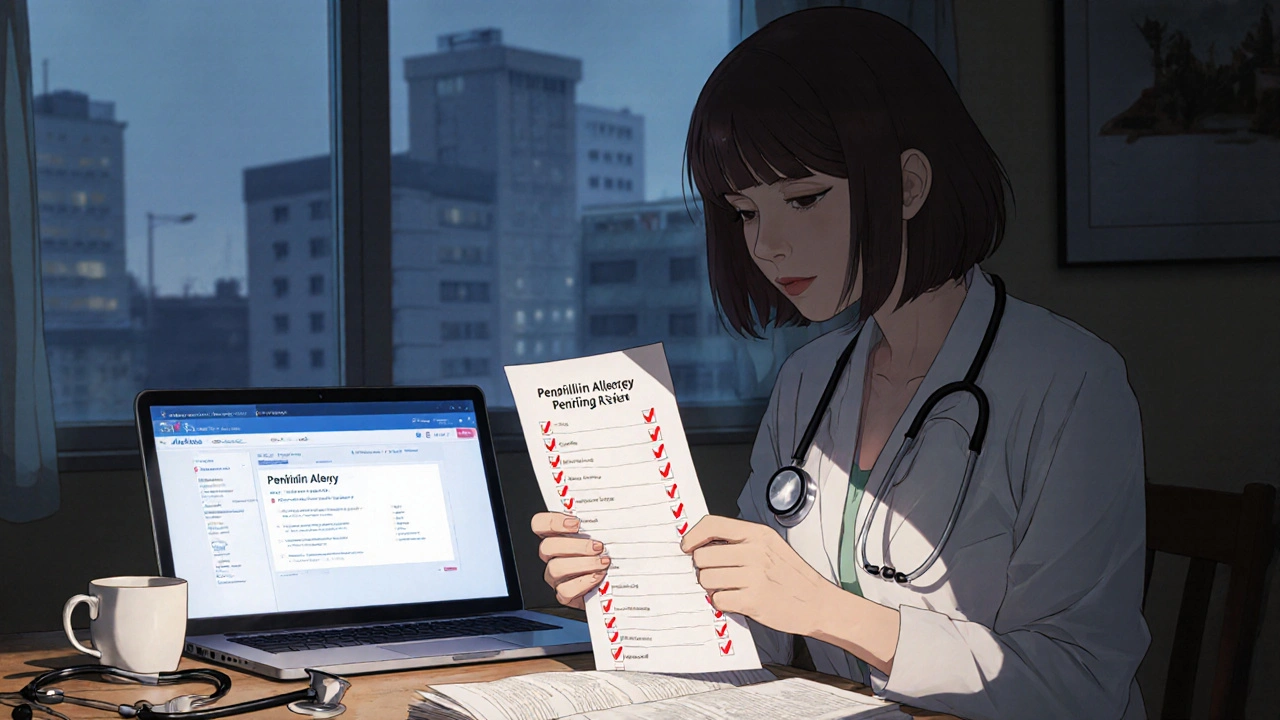
What a Correct Allergy List Should Include
Since January 1, 2025, U.S. healthcare systems are required by federal rule (USCDI v3) to document allergies in a specific way. Your allergy list shouldn’t just say “Penicillin allergy.” It needs:
- Exact drug name (e.g., “Amoxicillin,” not just “Penicillin”)
- Reaction description (e.g., “Hives and swelling within 30 minutes of dose”)
- Severity (Mild, Moderate, Severe, Anaphylactic)
- Timing (When did it happen? Days after? Right away?)
- Verification status (Patient-reported, Verified by provider, Confirmed by challenge test)
Without these details, a doctor might avoid all penicillin-class drugs-even if you’re only allergic to one. That’s why 68% of allergy discrepancies come from inconsistent documentation between specialists and your primary care provider.
How to Update Your Allergy List Yourself
You don’t have to wait for your doctor to catch up. Here’s how to take control:
- Review your current list-Log into your patient portal (MyChart, Epic, Cerner, etc.) and check what’s listed. If you don’t have access, call your primary care office and ask for a printed copy.
- Clarify every item-For each allergy, ask yourself: Did I ever have a true allergic reaction? Or was it nausea, dizziness, or a headache? If you’re unsure, write it down as “Possible reaction” and bring it up at your next visit.
- Request an allergy challenge test-If you’ve been told you’re allergic to penicillin but have taken it safely since, ask for a supervised skin test or oral challenge. It’s safe, quick, and covered by insurance. Studies show over 90% of people labeled “penicillin allergic” turn out not to be.
- Update your portal-Most portals let you submit updates. Use the “Message Your Doctor” feature. Don’t just say “I think I’m not allergic.” Say: “I believe my penicillin allergy is outdated. I took amoxicillin in 2023 with no reaction. I’d like to discuss a challenge test.”
- Bring your list to every appointment-Even if you updated it online, print it or show it on your phone. Providers still rely on paper charts in emergencies.
How Providers Should Be Updating Your List
Good clinics and hospitals now use advanced tools to catch errors before they hurt you. Systems like the one at Mass General Brigham use AI to scan your entire medical record-clinical notes, lab results, medication logs-and compare them to your official allergy list. If a doctor prescribed you amoxicillin last month and you didn’t react, the system flags it. It doesn’t just notify the doctor-it suggests removing the allergy label.
These systems can process 1,200 patient records per hour. Manual review? About 15 per hour. That’s why clinics with these tools reduced inappropriate antibiotic use by 24% and cut allergy alert overrides by 31%.
But not all systems are equal. Only 40% of U.S. hospitals have these advanced tools. If you’re going to a small clinic or rural hospital, don’t assume they’re checking. That’s why your active role matters.
What to Do When You Switch Providers
When you change doctors or move to a new city, your allergy list doesn’t automatically transfer. Even if the new provider uses the same EHR system, they might not have access to your old records unless you authorize it.
Here’s what to do:
- Request a copy of your full medical record, including allergies, before your first appointment.
- Ask the new provider to send a formal request to your old provider for EHR data transfer.
- If they use different systems (e.g., old: Epic, new: Cerner), ask if they use Care Everywhere or another interoperability tool. If not, hand them your printed list.
- At your first visit, say: “I’ve had issues with outdated allergy records before. Can we go over my list together and verify it?”
Patients who do this reduce their risk of being given a dangerous drug by 63%, according to a 2024 Mayo Clinic study.
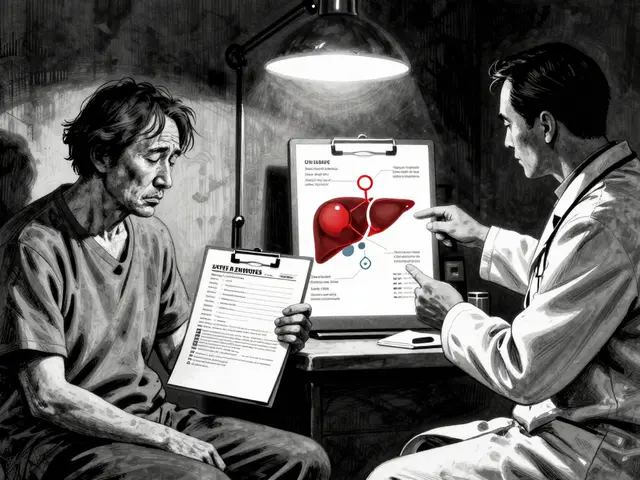
What’s Missing: Food and Environmental Allergies
Most EHRs are designed for drug allergies. They’re terrible at handling food or environmental ones. If you’re allergic to peanuts, shellfish, or bee stings, your allergy list might not even include it-or it might be buried in a clinical note.
Only 32% of major EHR systems accurately capture non-drug allergies. That’s a gap. So if you have food allergies, keep a separate card in your wallet or phone. Add it to your portal under “Other Allergies” if the system allows. And remind every provider: “I’m allergic to peanuts. Even trace amounts.”
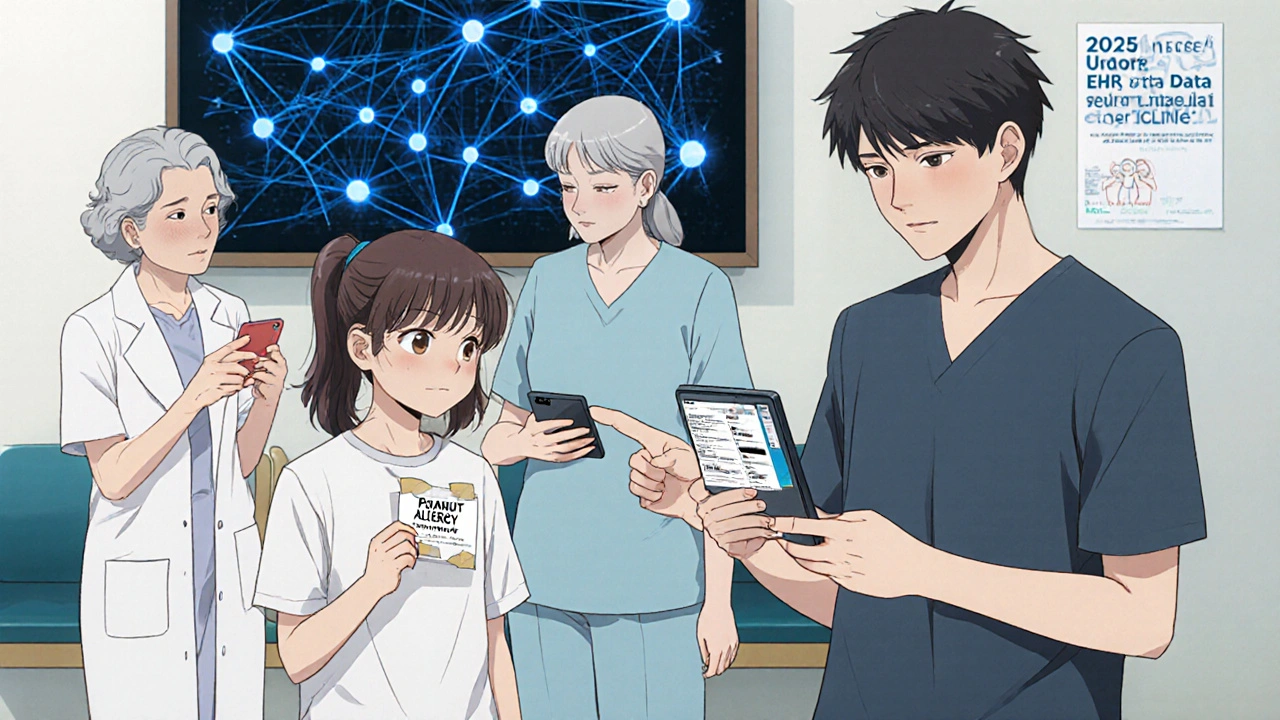
What’s Changing in 2025 and Beyond
Starting in 2026, Medicare will start penalizing hospitals if their allergy documentation is inaccurate. That means clinics are under pressure to fix this. New federal rules now let patients directly update their allergy records across providers using secure FHIR APIs-no paperwork needed. Think of it like updating your bank info online, but for your health data.
AI is getting smarter too. MIT’s 2024 prototype can predict if an allergy has resolved based on your medical history. If you haven’t had a reaction in 10 years and your immune markers are normal, the system can suggest removing the label.
But tech alone won’t fix this. Only 57% of doctors consistently use the reconciliation tools they have. That’s why your involvement is still the most powerful tool you have.
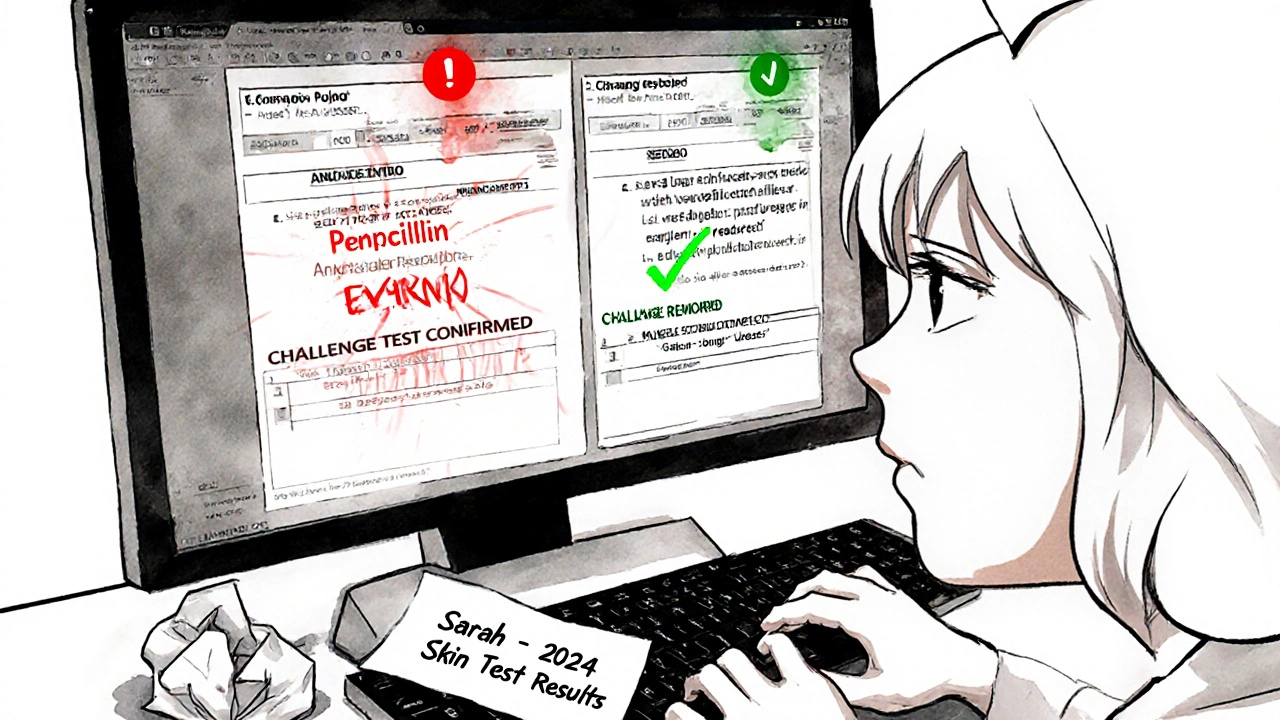
Real-World Example: Sarah’s Story
Sarah, 38, from Sydney, was told she was allergic to penicillin after a mild rash at age 10. She avoided all antibiotics for 28 years. In 2023, she got a serious sinus infection. Her GP prescribed azithromycin-more expensive, less effective, and harder on her gut. She asked: “Can I be tested?”
Her allergist did a skin test. Negative. Then an oral challenge. No reaction. Her allergy label was removed. The next time she got sick, she got amoxicillin. It worked in two days. Cost? $12. No side effects. Her insurance saved $1,100.
Sarah didn’t wait for the system to fix itself. She asked the question. She pushed for the test. She updated her portal. Now, every provider in her network has the correct record.
Final Checklist: Your Action Plan
Before your next appointment, do this:
- ✅ Check your patient portal for your current allergy list
- ✅ Cross-check each item with your memory-was it really an allergy?
- ✅ Write down any unclear reactions
- ✅ Ask your doctor if any allergies can be tested
- ✅ Update your portal with verified changes
- ✅ Print or screenshot your updated list
- ✅ Bring it to every new provider, even if you think they have it
There’s no app that will do this for you. No system is perfect. But you can be the one who makes sure your record is right. And that’s the most important thing.
What should I do if a provider won’t remove my allergy label?
If a provider refuses to remove an allergy label even after a confirmed negative challenge test, ask for a written explanation. You have the right to request your medical record be corrected under HIPAA and Australian Privacy Principles. If they still refuse, contact your health system’s patient advocate or file a formal request for amendment. Keep a copy of your test results and your written request.
Can I update my allergy list over the phone?
Some clinics allow phone updates for minor changes, but it’s not recommended. Verbal updates don’t get properly documented in your EHR. Always request updates in writing-through your patient portal, email, or a signed form. If you call, follow up with a message: “As discussed on [date], I’m requesting my penicillin allergy be removed based on my 2024 challenge test results.”
Are there apps that automatically update my allergies across providers?
Not yet. But starting in 2025, U.S. and Australian health systems are rolling out FHIR-based APIs that let you share your allergy list directly between providers using secure apps like MyHealthEData or My Health Record (Australia). You’ll be able to update once and push it to all connected clinics. For now, manual updates are still required-but this will change within the next two years.
How often should I review my allergy list?
Review it at least once a year, and always before any surgery, hospital admission, or new prescription. Allergies can change. You might outgrow one. Or you might develop a new one. Don’t assume your list is still accurate just because it hasn’t changed in years.
What if I have multiple allergies? How do I prioritize?
Label each one clearly by severity. Anaphylactic reactions go first. Then severe, moderate, mild. Use terms like “Life-threatening” or “Confirmed anaphylaxis.” Avoid vague labels like “Bad reaction.” Providers need to know what’s urgent. If you’re unsure, ask your allergist to help you rank them.




Kihya Beitz
November 14, 2025 at 14:45
So let me get this straight-I’m supposed to manually update my allergies across every system because doctors can’t be trusted to do their job? Cool. I’ll just spend my weekend playing medical admin instead of, idk, actually living my life.
Also, ‘penicillin allergy’ since age 8? Yeah, that’s not a mistake, that’s a feature. The system’s designed to scare doctors into prescribing expensive junk. I’m not surprised.