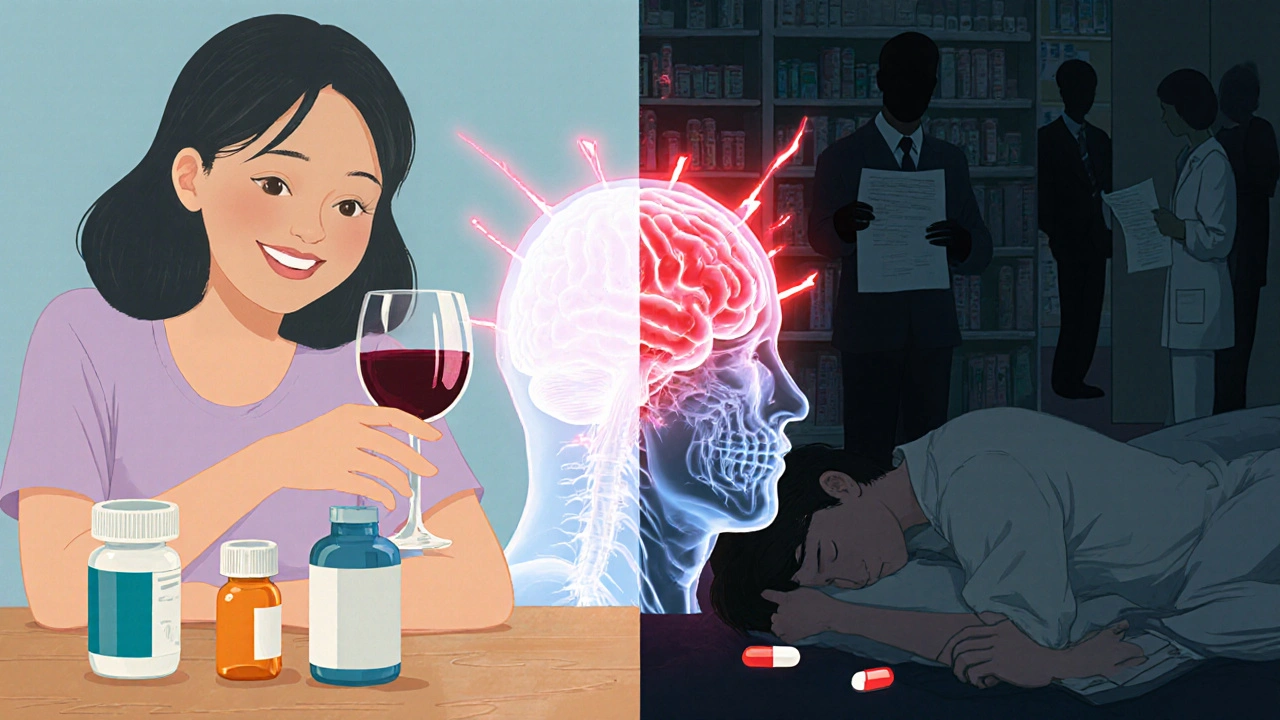
When you take one sedative, your body slows down a little. Take two, and it slows down more. But take three or four - especially if they’re from different classes - and your brain and lungs might stop working altogether. This isn’t a hypothetical risk. It’s happening right now, in homes, clinics, and emergency rooms across the country. Combining multiple sedatives isn’t just risky; it’s a silent killer that many people don’t even realize they’re playing with.
What Happens When Sedatives Combine?
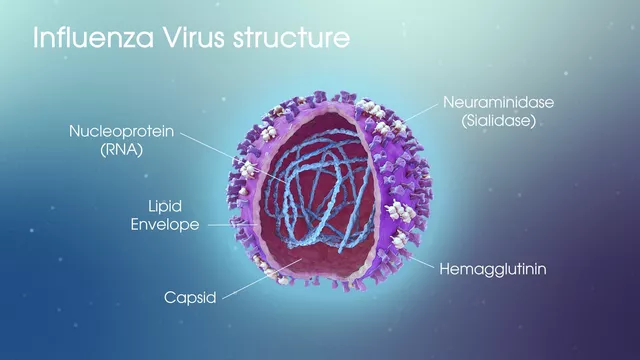
Sedatives like benzodiazepines (alprazolam, diazepam), opioids (oxycodone, hydrocodone), barbiturates, sleep pills (zolpidem), and even alcohol all do the same thing: they boost GABA, the brain’s main calming chemical. That’s why they help with anxiety, insomnia, or pain. But when you mix them, they don’t just add up - they multiply. This is called synergistic CNS depression. The result? Your breathing slows to dangerous levels. Your heart rate drops. Your blood pressure plummets. Your brain can’t tell your lungs to keep working.Studies show that when opioids and benzodiazepines are taken together, the risk of fatal overdose jumps by 2.5 to 4.5 times compared to opioids alone. In emergency rooms, 68% of patients who overdose on multiple sedatives show signs of confusion, dizziness, and severely slowed breathing - often as low as 8 to 10 breaths per minute. Normal is 12 to 20. When it drops below 6, oxygen levels crash. Brain damage can start in as little as four minutes. Death isn’t far behind.
Who’s Most at Risk?
This isn’t just about street drug users. It’s happening to people who follow their prescriptions. Elderly patients are especially vulnerable. A 75-year-old taking lorazepam for anxiety, oxycodone for back pain, and zolpidem for sleep is already on a dangerous cocktail. Studies show these patients are 2.8 times more likely to fall and 3.4 times more likely to suffer a hip fracture. That’s not just about dizziness - it’s about their brain being too sedated to react to a stumble.Women are at higher risk too. Research shows they’re 1.7 times more likely to be prescribed multiple sedatives than men. People with depression are 2.1 times more likely to be on this dangerous combo. And if you’ve struggled with substance use before, your odds of mixing sedatives jump from 29% to 39%. Even worse - 12 to 13% of those on opioids drink alcohol within two hours of taking their pill. That’s like lighting a match near gasoline.
The Long-Term Toll
Most people think the danger is only in the moment - an overdose. But the damage builds slowly. Long-term users of multiple sedatives report chronic fatigue in 45% of cases. Weight gain? Averaging 12 to 18 pounds in a year. Sexual dysfunction? Affects 32%. Sleep apnea? 27% develop it. Depression? 38%. Suicidal thoughts? 19% report them after just six months.And it’s not just physical. Cognitive decline is real. A major study found that elderly patients on multiple CNS depressants had a 27% higher chance of losing five or more points on a standard memory test. That’s not normal aging. That’s drug-induced brain fog. And once it starts, it doesn’t always reverse - even after stopping the drugs.

The Worst Combinations
Some mixes are deadlier than others. Here are the top three most dangerous combinations, backed by clinical data:- Opioid + Benzodiazepine - The most lethal combo. Responsible for the majority of fatal overdoses involving prescription drugs. The FDA issued a formal warning in 2016 after hundreds of deaths were linked to this mix.
- Opioid + Alcohol - Even one drink with an opioid can drop your breathing rate below 10 breaths per minute. No safe amount exists.
- Benzodiazepine + Sleep Medication - Mixing diazepam with zolpidem doesn’t make you sleep better - it makes you stop breathing while asleep. Many don’t wake up.
Even antidepressants like SSRIs can make things worse. They interfere with how your liver breaks down sedatives, causing them to build up in your system. One study found that nearly 70% of hospitalizations for depression involved patients on multiple CNS-acting drugs - with almost no clear guidance from doctors on how dangerous that was.
Why Do Doctors Still Prescribe These Combos?
It’s not because they’re careless. It’s because the system is broken. Pain patients get opioids. Anxiety patients get benzodiazepines. Insomnia patients get sleep pills. No one connects the dots. Many doctors don’t even know the Beers Criteria - a list of medications that should be avoided in older adults because of their risks. Only 28% of clinics use electronic systems that flag dangerous combinations automatically.And patients? They don’t always tell their doctors everything. They might not mention the wine they have at dinner. Or the Xanax they take for panic attacks. Or the leftover hydrocodone they keep in the medicine cabinet. By the time someone ends up in the ER, it’s too late to ask.
What Can You Do?
If you or someone you care about is on more than one sedative, here’s what to do now:- Make a full list - Write down every pill, liquid, or patch you take, including over-the-counter sleep aids and alcohol.
- Ask your doctor - Say: “Am I on any drugs that could dangerously interact? Could any be removed?”
- Request a medication review - Every 3 to 6 months, ask for a formal deprescribing plan. Studies show this cuts fall risk by 32% and cognitive decline by 27%.
- Use a pharmacy checker - Most pharmacies now have systems that flag dangerous combos. Ask your pharmacist to run a check.
- Never mix with alcohol - Not even one drink. Not even on special occasions.
There are safer alternatives. For anxiety, cognitive behavioral therapy (CBT) works as well as benzodiazepines - without the risk. For sleep, improving sleep hygiene cuts insomnia by 60% in most cases. For pain, physical therapy, nerve blocks, or non-opioid meds like gabapentin often do the job without the danger.
The Future Is Changing - But Not Fast Enough
The FDA’s 2016 warning was a wake-up call. The CDC’s guidelines led to a 15% drop in co-prescribing between 2014 and 2018. But in 2020, over 10% of patients on long-term opioids were still getting benzodiazepines - despite the warnings. That’s 1 in 10 people still on the edge.Technology is catching up. By 2025, most electronic health records will automatically block dangerous combinations unless a doctor overrides the alert. Some hospitals are already using genetic testing to find people who metabolize drugs slowly - these patients are 22% more likely to overdose on standard doses. Personalized medicine is coming. But it’s not here yet.
Right now, the only thing that can save you is awareness. If you’re on more than one sedative, you’re not being careful - you’re playing Russian roulette with your breathing. And the gun is loaded.
Can you die from mixing just two sedatives?
Yes. Even two sedatives - like an opioid and a benzodiazepine - can cause fatal respiratory depression. The risk is 2.5 to 4.5 times higher than using either drug alone. You don’t need to take four or five to die. One dangerous combo is enough.
Is it safe to take a sleep aid with my anxiety medication?
No. Sleep aids like zolpidem and anxiety meds like alprazolam both act on GABA receptors. Together, they can suppress your breathing to life-threatening levels, especially at night when your body is already relaxed. Many people die in their sleep from this combo without anyone realizing what happened.
What should I do if I accidentally took multiple sedatives?
Call emergency services immediately. Don’t wait for symptoms. Signs like slow breathing, confusion, unresponsiveness, or blue lips mean your body is shutting down. Even if you feel fine, the effects can build over hours. Do not try to sleep it off. This is a medical emergency.
Can my doctor just stop my sedatives cold turkey?
No. Stopping sedatives suddenly - especially after long-term use - can cause seizures, hallucinations, or even death. Any reduction must be gradual and supervised. Ask your doctor for a tapering plan. Never adjust doses on your own.
Are natural remedies like melatonin or valerian root safer?
Melatonin is generally low-risk and doesn’t cause CNS depression. Valerian root has mild sedative effects but rarely causes serious issues on its own. However, combining them with prescription sedatives can still increase drowsiness and impair coordination. Always tell your doctor about supplements - they’re not harmless just because they’re “natural.”
How do I know if I’m dependent on sedatives?
If you feel anxious, shaky, or have trouble sleeping without your meds - or if you’ve increased your dose over time - you may be dependent. Physical dependence doesn’t mean addiction, but it does mean your body needs the drug to function normally. Talk to your doctor. You’re not weak. You’re human.



Scott Collard
November 30, 2025 at 21:47
This isn’t just medical advice-it’s a public health emergency masked as routine care. Doctors are prescribing like it’s a buffet and patients are dying at the table. No one’s holding them accountable.
And don’t get me started on the pharmacies that just fill the script without a second thought. If your system doesn’t flag a benzo-opioid combo, it’s broken. Not negligent-broken.
Someone needs to sue the AMA for enabling this.