When you take a pill, inject a vaccine, or use a medical device, you expect it to be safe, effective, and consistent. That’s not luck. It’s the result of Current Good Manufacturing Practice (GMP) standards - the backbone of quality in pharmaceuticals, medical devices, and even some food products. These aren’t suggestions. They’re legally enforceable rules that keep dangerous mistakes from reaching patients. And as of 2026, those rules have changed significantly.
What Exactly Are Current GMP Standards?
Current GMP, often written as cGMP, is a set of regulations that require manufacturers to use modern systems, up-to-date technology, and proven processes to ensure product quality. The "C" stands for "current" - meaning you can’t rely on old methods just because they worked in the past. If a better way exists, you must adopt it.
The U.S. FDA first codified these rules in 1978 under 21 C.F.R. Parts 210 and 211, but they’ve been updated constantly. In 2023, the FDA issued new guidance on testing high-risk ingredients like glycerin for contaminants. In January 2025, they clarified that manufacturers can use in-line sensors instead of physically pulling samples for testing - as long as the method is scientifically validated. That’s a major shift from traditional lab testing.
The European Union’s rules, found in EudraLex Volume 4, are stricter in some areas. Their Annex 1 update, fully active since August 2024, demands closed isolator systems for sterile manufacturing. That means no human hands can touch sterile products during filling - a huge change from open laminar airflow hoods used for decades.
WHO GMP standards serve as a baseline for low- and middle-income countries, but they lack enforcement power. While the FDA and EMA can shut down a factory, WHO can only recommend. As of 2024, only 43% of facilities in emerging markets met even basic WHO GMP requirements.
The Nine Core Requirements of GMP in 2026
Every compliant facility must meet these nine pillars. Missing one can trigger a warning letter, a product recall, or worse - a factory shutdown.
- Quality Management: You need a full quality system that covers everything - from raw materials to final shipping. The quality unit must have authority to stop production if something’s off. No exceptions.
- Sanitation and Hygiene: Clean rooms aren’t optional. For sterile products, air must meet ISO 14644-1 Class 5 standards - that’s 3,520 particles per cubic meter or less. Cleaning procedures must be validated and documented. No guesswork.
- Building and Facilities: Layout matters. You can’t have raw materials and finished products sharing the same hallway. Airflow must be controlled, pressure differentials maintained, and environmental monitoring continuous. Temperature and humidity logs? Required daily.
- Equipment: Every machine must go through IQ (Installation Qualification), OQ (Operational Qualification), and PQ (Performance Qualification). If you replace a pump, you don’t just install it - you prove it works correctly under real conditions. The FDA requires this under § 211.67.
- Raw Materials: Every batch of active ingredient must be tested for identity, purity, and strength before use. Suppliers must be approved. Storage conditions must be monitored. If a container of lactose sits in a hot warehouse for a week, it’s not fit for use.
- Personnel: Training isn’t a one-time event. Staff must be trained quarterly on GMP basics, specific procedures, and hygiene. Competency checks are mandatory. If someone doesn’t pass, they can’t touch product.
- Validation and Qualification: You must prove your process works consistently. Batch-to-batch variation? Not allowed. Process validation must be documented, reviewed by quality, and updated when changes occur. The FDA’s January 2025 guidance says you can’t rely on models alone - you need real-time data to back them up.
- Complaints and Recalls: If a patient reports a problem, you have 72 hours to investigate. Root cause analysis must be done. Recalls must be swift and traceable. EMA reported that 18% of 2024 recalls were due to poor supply chain oversight - meaning the problem started with a supplier you didn’t properly vet.
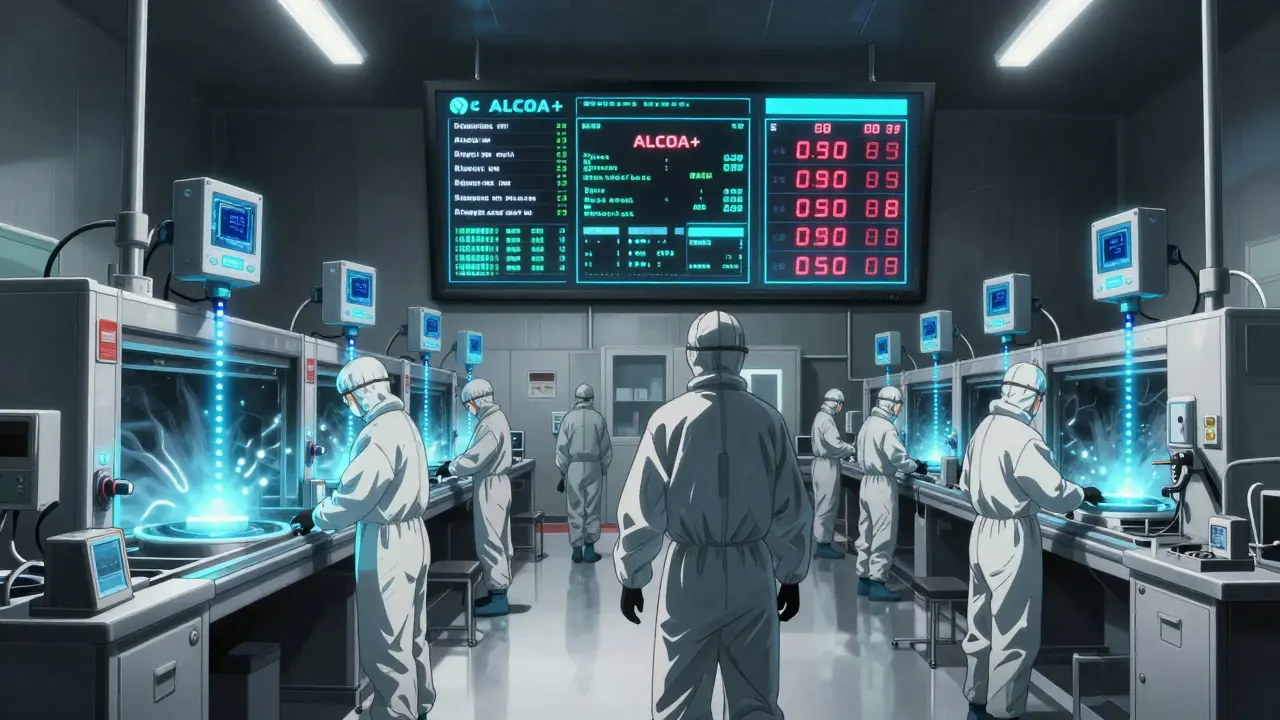
- Documentation and Record Keeping: If it wasn’t written down, it didn’t happen. All records must be contemporaneous - written at the time of the activity. Electronic records must follow ALCOA+ principles: Attributable, Legible, Contemporaneous, Original, Accurate, and Complete, Consistent, Enduring, Available. Audit trails are required for every change.
FDA vs. EU GMP: Key Differences You Can’t Ignore
Global companies don’t just need to comply - they need to navigate two very different rulebooks.
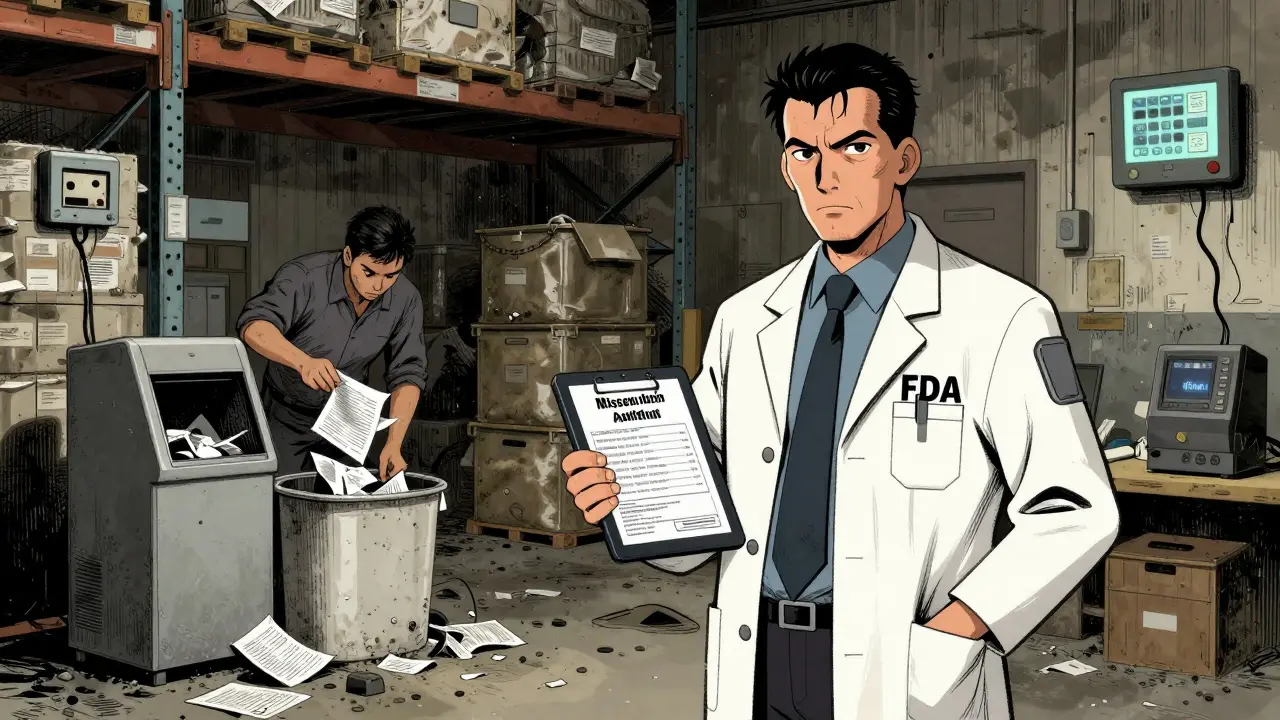
The FDA gives you flexibility. You can choose your own methods as long as they’re scientifically sound. That’s great if you’re innovative. But it also means inspectors have more room to interpret your choices - and 2,147 warning letters were issued in FY2024 for data integrity violations.
The EU is more prescriptive. Annex 1 tells you exactly how to gown, how to monitor air, and how to design isolators. It’s clearer - but harder to adapt to. One Pfizer supervisor reported spending $75,000 a year just to run duplicate environmental tests because FDA and EU requirements don’t fully align.
Here’s where they differ most:
| Requirement | FDA (2025) | EU GMP Annex 1 (2024) |
|---|---|---|
| Sampling for Testing | Allows in-line, at-line, or on-line measurements | Still requires physical sampling for critical attributes |
| Sterile Gowning | Recommended best practices | Mandatory full-body sterile garments with no exposed skin |
| Data Integrity | ALCOA+ enforced strictly; audit trails required | ALCOA+ required; electronic systems must have validated audit trails |
| Process Models | Must be paired with in-process testing | Accepted if validated with physical data |
| Enforcement | High volume of warning letters; flexible interpretation | Fewer letters, but higher chance of shutdowns |
Market share reflects this: 34% of global pharma production follows FDA rules, 28% follow EU rules. The rest mostly follow WHO standards - but with inconsistent oversight.
What’s Changing in 2026?
Three big trends are reshaping GMP compliance right now.
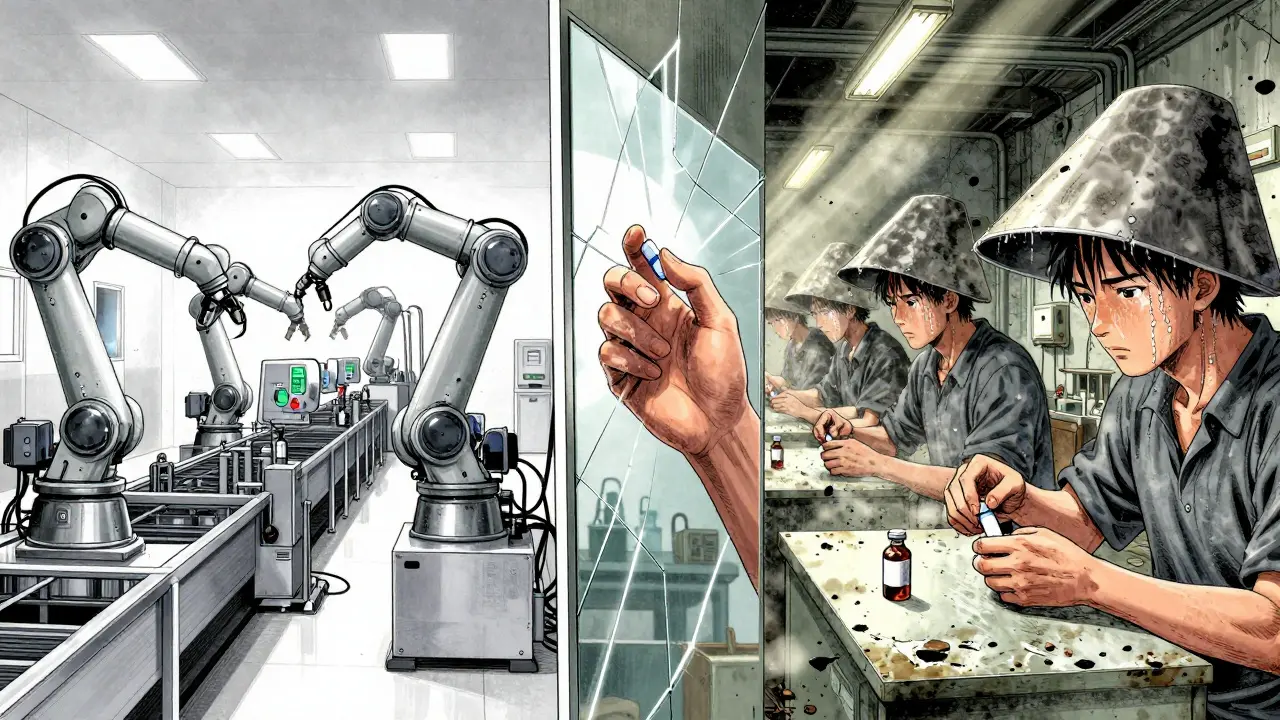
1. Advanced Manufacturing Is Now the Norm
Continuous manufacturing - where products are made in one long, uninterrupted process instead of in batches - jumped 37% from 2023 to 2025. Companies like Merck have achieved zero FDA 483 observations by using Process Analytical Technology (PAT) tools that monitor quality in real time. No more waiting for lab results. If the pH drops, the system adjusts automatically.
2. Data Integrity Is the #1 Compliance Challenge
A PharmaTech survey of 347 facilities found 68% of respondents struggled with data integrity. That means falsified logs, missing audit trails, or back-dated entries. Remediation costs averaged $185,000 per facility. The FDA’s focus here is relentless. If your system doesn’t track who changed what and when, you’re at risk.
3. Supply Chain Oversight Is Tightening
Both FDA and EMA now require risk-based supplier audits. You can’t just take a certificate from a vendor. You must assess their GMP compliance. In 2024, 27% of recalls traced back to supplier issues. That’s not just a quality problem - it’s a legal liability.
Implementation: What It Really Costs and How Long It Takes
Compliance isn’t a project you finish in six months. It’s a culture.
For a mid-sized pharma plant, full GMP compliance takes 18 to 24 months. Costs? Around $1.2 million on average. That includes:
- Hiring a dedicated compliance team (minimum 3 full-time staff for facilities over 10,000 sq ft)
- Writing 120-150 standard operating procedures (SOPs)
- Training staff 40+ hours per year
- Upgrading equipment for qualification and automation
- Installing environmental monitoring systems
- Validating new software for electronic records
Legacy equipment is the biggest headache. One Quality Assurance Manager on Reddit said integrating in-line sensors into old production lines cost $250,000 per line. And that’s just the hardware - validation adds more.
Resistance to documentation is another silent killer. Over 60% of FDA 483 observations in 2024 cited poor record-keeping. People think it’s paperwork. It’s legal protection.
What Happens If You Don’t Comply?
Non-compliance doesn’t just mean a fine. It means:
- Product recalls - expensive, damaging to reputation
- Import bans - your product can’t enter the U.S. or EU
- Factory shutdowns - regulators can close your facility
- Criminal charges - for intentional fraud or falsified data
In 2024, the FDA issued over 2,000 warning letters. Many led to consent decrees - court-enforced agreements that require third-party audits and monthly reporting for years.
There’s no such thing as "almost compliant." If your audit trail is missing, your training records are incomplete, or your cleaning validation is outdated - you’re non-compliant. Period.
How to Stay Ahead
Don’t wait for an inspection to start fixing things. Here’s what works:
- Map your entire process - from raw material receipt to final shipment. Find every point where quality can break.
- Invest in automation - especially for data collection. Manual entry is your biggest risk.
- Train constantly. Make GMP part of daily conversation, not just annual training.
- Use risk-based approaches (ICH Q9). Focus resources where the real danger lies.
- Build relationships with regulators. Attend FDA and EMA workshops. Ask questions before you’re in trouble.
The goal isn’t just to pass an audit. It’s to build a system so reliable that you never have to worry about one.
Is GMP only for pharmaceuticals?
No. While GMP is most strictly enforced in pharmaceuticals, it also applies to medical devices, dietary supplements, and in some countries, food products. The FDA regulates dietary supplements under 21 C.F.R. Part 111, which is based on GMP principles. The EU has similar rules for food contact materials and supplements. The core goal is the same: prevent contamination, mix-ups, and errors.
Can I use cloud-based software for GMP records?
Yes - but only if it’s validated. The FDA and EU require that electronic systems are secure, have audit trails, and prevent unauthorized changes. You can’t just use Google Sheets or Dropbox. You need software designed for regulated environments, with features like role-based access, electronic signatures, and automated backups. Validation must prove it works as intended under real conditions.
How often are GMP inspections conducted?
The FDA inspects high-risk facilities every 2-3 years. Lower-risk ones may be inspected every 4-5 years. The EU follows a risk-based schedule too, but inspections are more frequent for sterile manufacturers. WHO doesn’t inspect directly - it relies on national regulators. However, if you export to the U.S. or EU, you’ll be inspected by their teams, even if you’re based overseas.
What’s the biggest mistake companies make with GMP?
Thinking compliance is a checklist. GMP isn’t about ticking boxes. It’s about culture. The biggest failures happen when quality is seen as a department, not a company-wide responsibility. If production staff skip documentation to meet deadlines, or managers ignore deviations because "it’s never caused a problem," you’re already non-compliant. GMP only works when everyone owns it.
Do small companies need full GMP compliance?
Yes - if they’re manufacturing products for sale. Size doesn’t matter. Even a small lab making custom compounded prescriptions must follow GMP rules. The FDA doesn’t exempt small businesses. The only exceptions are for certain over-the-counter products or in-house use under specific conditions. But if you’re selling to pharmacies or hospitals, you’re regulated. Start small, but start right.
What’s the future of GMP?
The future is real-time quality. AI-driven systems will predict defects before they happen. Sensors will monitor every step of production. Paper records will vanish. But the core principle won’t change: you must prove your product is safe and consistent. The rules will evolve to match the technology, but the goal - protecting patients - stays the same. Companies that embrace digital transformation now will lead the next decade. Those that wait will be left behind.




Stephen Rock
January 20, 2026 at 22:48
GMP is just corporate theater. They spend millions on audit trails while the actual product quality is decided by a spreadsheet someone filled out at 2 a.m. I’ve seen it. The system’s broken.