When you take a pill, you expect it to help - not hurt. But sometimes, medications cause side effects. Some are predictable. Others come out of nowhere. The difference between these two kinds of reactions isn’t just academic - it changes how doctors treat you, what drugs they avoid, and even whether you can safely take a medicine again.
What Are Dose-Related Side Effects?
Dose-related side effects, also called Type A reactions, happen because the drug is doing exactly what it’s supposed to do - just too much. Think of it like turning up the volume on a speaker: the sound gets louder, but it’s still the same song. These reactions are predictable, common, and directly tied to how much of the drug is in your body.
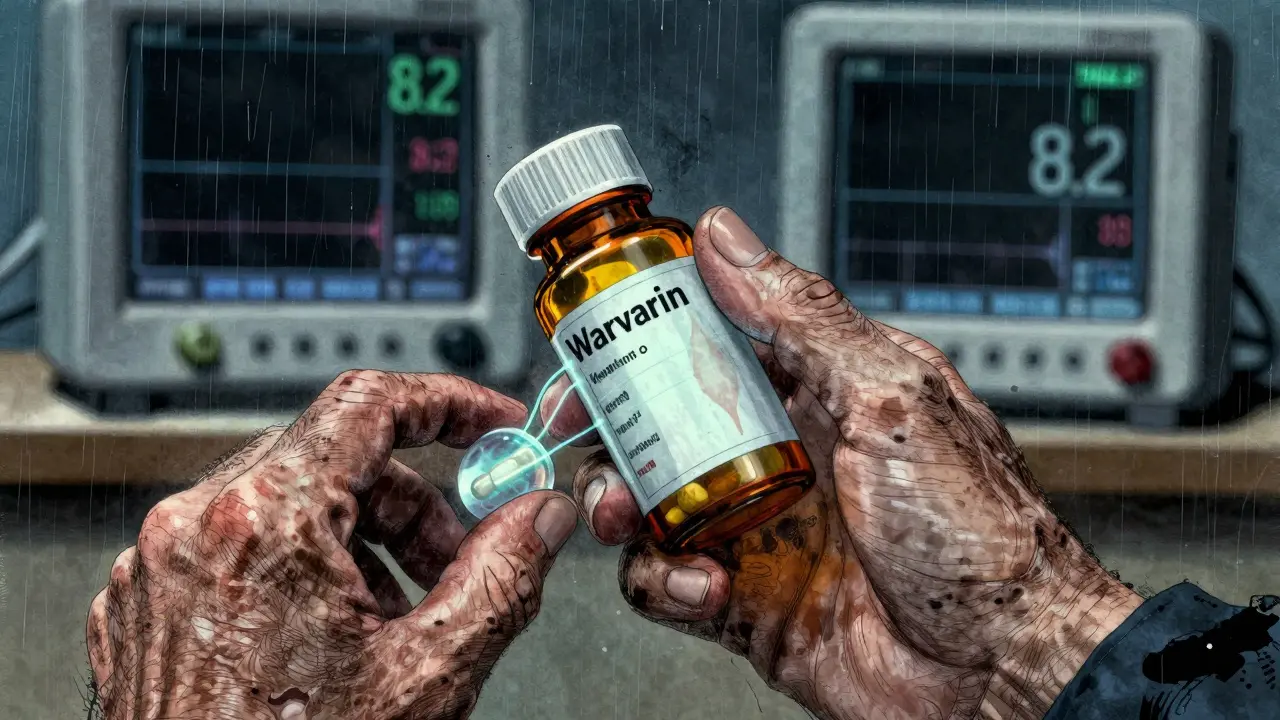
Examples are everywhere. If you’re on warfarin to thin your blood, and your INR jumps to 8.2 after starting another antibiotic, that’s a dose-related reaction. The antibiotic interferes with how your body breaks down warfarin, causing too much blood thinning. Same with insulin: take too much, and your blood sugar crashes below 70 mg/dL. Or take too much lithium for bipolar disorder, and you get tremors, confusion, or even seizures - because the drug’s safe range is razor-thin (0.6-1.0 mmol/L), and toxicity starts above 1.2 mmol/L.
These reactions make up 70-80% of all adverse drug reactions. They’re the reason doctors monitor blood levels for drugs like digoxin, vancomycin, and phenytoin. They’re also why kidney or liver problems change your dosing. If your kidneys aren’t clearing metformin properly, you risk lactic acidosis. If your liver can’t process diazepam, you’ll feel drowsy for days. These aren’t accidents - they’re extensions of the drug’s known effects, made worse by your body’s ability (or inability) to handle the dose.
What Are Non-Dose-Related Side Effects?
Non-dose-related side effects, or Type B reactions, are the opposite. They’re unpredictable, rare, and don’t follow the rules of pharmacology. You could take one pill and have a life-threatening reaction. Someone else takes ten times that dose and feels fine. It’s not about the amount - it’s about your body’s unique response.
The most dramatic examples are allergic or immune-driven reactions. Anaphylaxis after penicillin. Stevens-Johnson syndrome from lamotrigine. Drug-induced liver injury from amoxicillin-clavulanate. These don’t happen because you took too much. They happen because your immune system mistakes the drug for a threat. Once your body has been sensitized - even from a past exposure - it reacts violently, often with the first dose of a new course.
These reactions are rare - only 15-20% of all side effects - but they cause 70-80% of serious hospitalizations and drug-related deaths. Why? Because they’re sudden. They don’t give you warning signs. You can follow every dosing guideline perfectly and still end up in the ER with a blistering skin rash or liver failure.
And here’s the twist: even these “non-dose-related” reactions may have hidden thresholds. Some people can tolerate a tiny dose of a drug without issue, while others react to a single tablet. The problem is, those thresholds vary wildly between individuals. So in population studies, they look random. But for you, the threshold might be exactly one pill.
Why the Distinction Matters in Real Life
This isn’t just textbook stuff. It changes your treatment plan.
If you have a Type A reaction - say, low blood pressure from an antihypertensive - your doctor will lower the dose. Maybe switch you to a different drug in the same class. They’ll monitor your numbers. You might need regular blood tests. The goal? Find the sweet spot where the drug works without overdoing it.
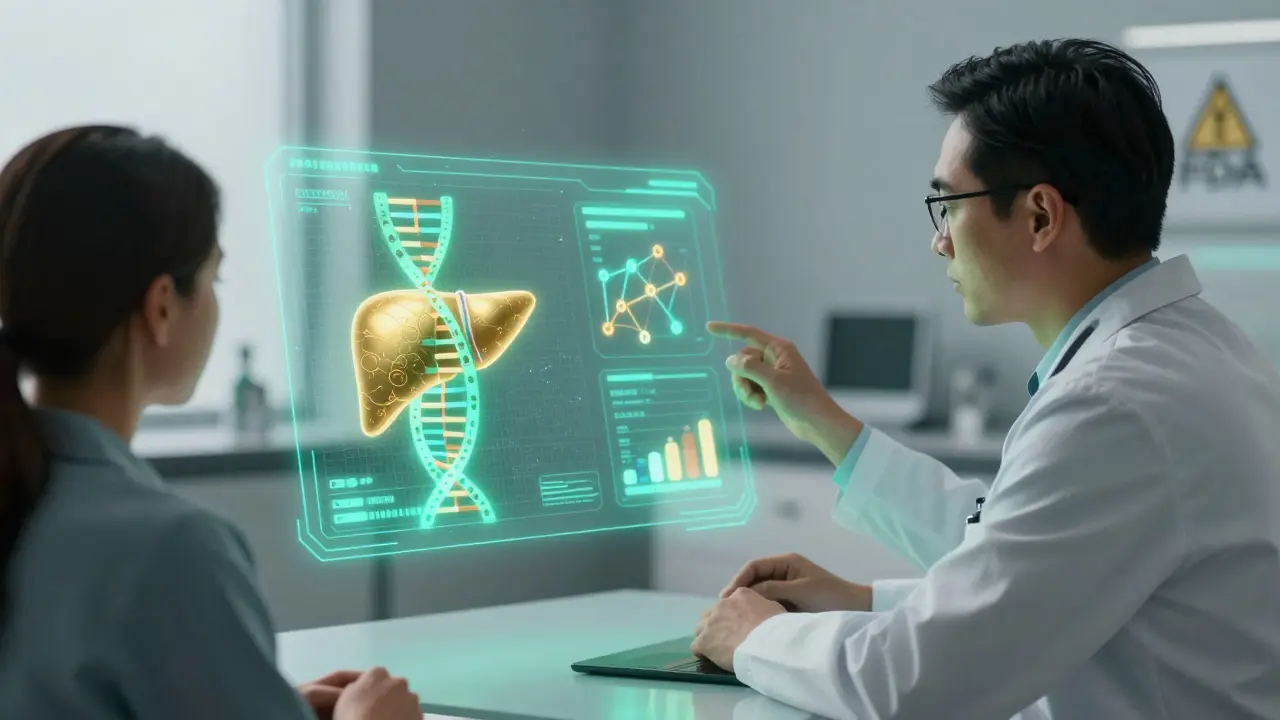
But if you have a Type B reaction - like a severe rash from carbamazepine - the answer is simple: stop it forever. No dose adjustment. No second chance. You can’t take it again. And you can’t take similar drugs either. That’s why doctors now test for HLA-B*15:02 before giving carbamazepine to patients of Asian descent. If you have that gene, your risk of Stevens-Johnson syndrome jumps from less than 1 in 10,000 to nearly 1 in 10. The test costs $215. The cost of missing it? Death or permanent scarring.
Same with abacavir for HIV. HLA-B*57:01 screening cuts hypersensitivity reactions from 8% to under 0.5%. That’s not just good medicine - it’s life-saving precision.

Who’s Most at Risk?
Older adults are hit hardest by Type A reactions. Why? Their kidneys and liver don’t clear drugs as well. Their bodies hold onto medication longer. A 70-year-old on warfarin or insulin is far more likely to have a dangerous drop in blood pressure or blood sugar than a healthy 30-year-old. In fact, 67% of emergency visits for drug side effects in people over 65 are caused by anticoagulants, insulin, and oral diabetes drugs - all classic Type A offenders.
Type B reactions can strike anyone, but they’re more common in people with certain genetic traits. HLA genes are the biggest red flag. HLA-B*57:01 for abacavir. HLA-B*15:02 for carbamazepine. HLA-A*31:01 for phenytoin. These aren’t random. They’re inherited. That’s why genetic testing is becoming standard before prescribing certain drugs - especially in populations where the risk is higher.
Drug interactions also boost Type A risk. Clarithromycin can make statin levels spike by 5-10 times. That’s not an allergy. That’s a pharmacokinetic collision. Your liver can’t process both drugs at once. The result? Muscle damage, kidney failure, even rhabdomyolysis.
How Doctors Prevent and Manage These Reactions
For Type A reactions, prevention is all about control:
- Therapeutic drug monitoring - checking blood levels of digoxin, vancomycin, lithium
- Dose adjustments based on kidney or liver function
- Avoiding drug combinations that interfere with metabolism (like grapefruit juice with statins)
- Using dosing algorithms for warfarin based on age, weight, and genetics
For Type B reactions, prevention is about avoiding the trigger entirely:
- Genetic screening before prescribing high-risk drugs
- Skin testing for penicillin allergy (50-70% accurate)
- Graded challenges - slowly reintroducing a drug under supervision if you have a low-risk history
- Black box warnings and REMS programs - strict controls required by the FDA for drugs like clozapine and isotretinoin
One study showed that hospitals using Type A prevention protocols reduced major bleeding in warfarin patients by 35%. That’s not a small win - it’s hundreds of lives saved every year.
The Future: Personalized Dosing and Predictive Tools
The field is moving fast. The global pharmacogenomics market is set to hit $17.9 billion by 2030. Why? Because we’re learning how to predict who will react - and how.
The FDA now lists pharmacogenomic info on 311 drug labels. Twenty-eight of them require genetic testing before use. Companies are building AI tools that scan electronic health records to spot early signs of Type A reactions with 82% accuracy. But Type B? Only 63%. That’s the challenge - immune reactions are still a black box.
What’s coming next? Dosing software that combines your DNA, your age, your kidney function, your current meds, and your history to calculate your perfect dose - not just for effectiveness, but for safety. The FDA is already drafting guidelines for this kind of tool. It’s not science fiction. It’s the next step in making medicine safer for everyone.
What This Means for You
If you’re on medication, know this: side effects aren’t all the same. Some mean you need a lower dose. Others mean you need to stop completely. Don’t assume a reaction is “just a side effect” - ask your doctor which type it is.
Did you get a rash after starting a new drug? Ask: Was it dose-dependent? Did it happen right away? Did anyone else you know have the same reaction? That tells you whether it’s Type A or Type B.
And if you’ve had a serious reaction before - especially one that came out of nowhere - make sure your medical records reflect it. Carry a list of drugs you can’t take. Talk to your pharmacist. Ask about genetic testing if you’re being prescribed a high-risk drug.
Medicine is getting smarter. But you’re still the most important part of the equation. Knowing the difference between dose-related and non-dose-related side effects gives you power - the power to ask the right questions, make informed choices, and stay safe.