Statin Tolerance Calculator
Personalized Statin Recommendation Tool
Based on SLCO1B1 genetic testing results and CPIC guidelines, this tool helps determine which statins may be safer for you.
Your Statin Tolerance Risk
Low RiskSafer Alternatives:
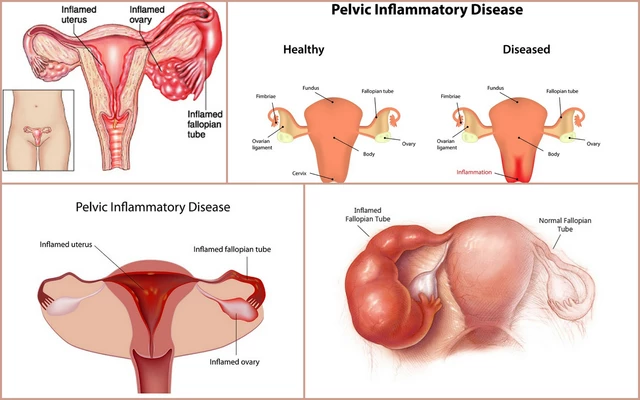
Millions of people take statins to lower cholesterol and prevent heart attacks. But for up to 1 in 3 of them, the side effects-especially muscle pain, weakness, or cramps-are bad enough to make them quit. Often, doctors assume it’s just a coincidence, or blame the patient for being overly sensitive. But what if the real issue isn’t your body being weak-it’s your genes?
Why Some People Can’t Tolerate Statins
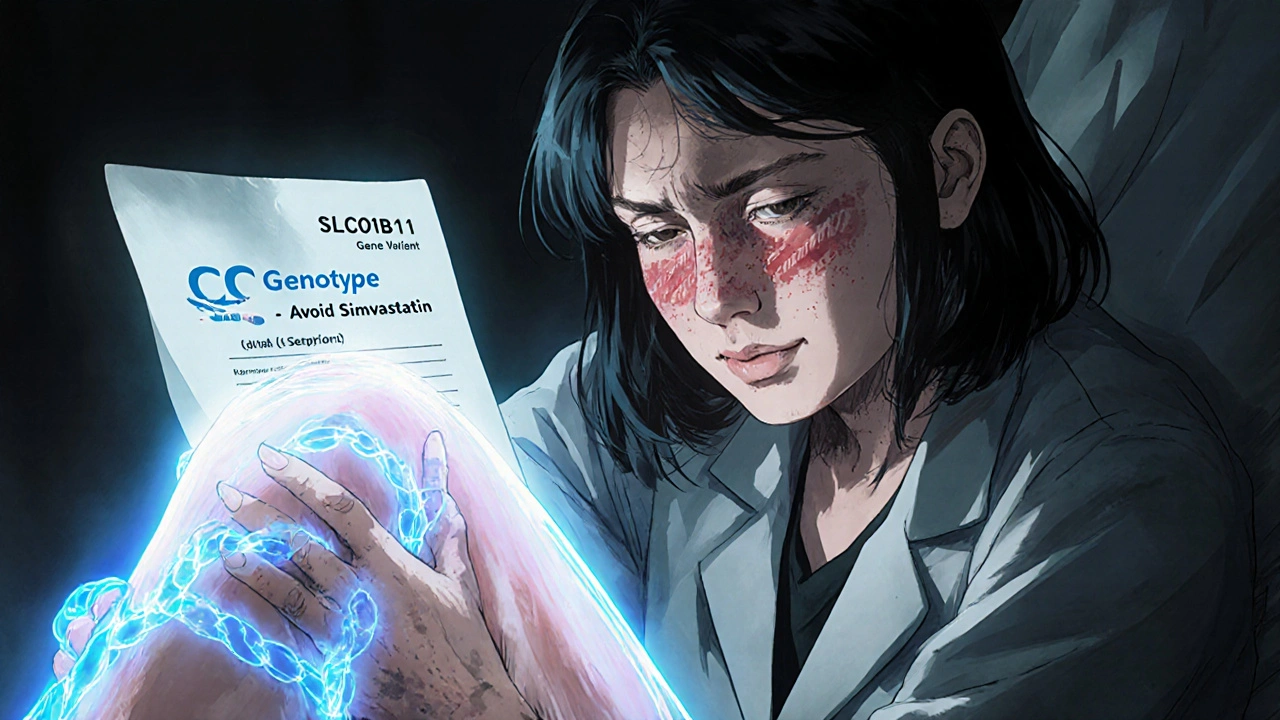
Statin-induced muscle symptoms (SAMS) are the #1 reason people stop taking these life-saving drugs. The problem isn’t always dose or age. In fact, two people on the same statin, at the same dose, with identical health histories, can have wildly different experiences. One feels fine. The other can’t walk up the stairs without aching. That’s where genetics come in. The key player is a gene called SLCO1B1 a gene that codes for a liver protein responsible for pulling statins out of the bloodstream and into the liver where they work. A common variant, rs4149056 (also called the C allele), makes this protein less effective. When that happens, statins build up in your muscles instead of being cleared properly. That’s what causes the pain. If you have two copies of the C variant (CC genotype), your risk of severe muscle damage from simvastatin is nearly five times higher than someone with the normal TT version. About 1-2% of people of European descent fall into this high-risk group. Another 15% carry one copy (TC), putting them at moderate risk. These numbers don’t change based on diet, exercise, or how hard you work out. It’s written in your DNA.Not All Statins Are Created Equal
This is where things get practical. The SLCO1B1 gene issue matters most for simvastatin a statin that relies heavily on the OATP1B1 transporter to enter the liver. If you’re on simvastatin 80mg and have the CC genotype, you’re in serious danger of rhabdomyolysis-a rare but dangerous breakdown of muscle tissue. But here’s the good news: not all statins are affected the same way. pravastatin a statin that doesn’t depend on SLCO1B1 for liver uptake and fluvastatin another statin with minimal reliance on the OATP1B1 transporter work just fine even if you have the risky gene variant. Studies show pravastatin causes 80% fewer muscle problems in CC genotype carriers compared to simvastatin. The same goes for atorvastatin a statin metabolized primarily by CYP3A4, not SLCO1B1 and rosuvastatin a statin with low dependence on the SLCO1B1 transporter. Large studies, including one with nearly 12,000 participants, found no link between SLCO1B1 variants and muscle symptoms for these two drugs. So if you’ve been told you’re "statin intolerant," you might just be intolerant to the wrong statin.Who Should Get Tested?
You don’t need to be genetically tested if you’ve never had muscle pain on statins. But if you’ve tried one statin and quit because of muscle aches, testing makes sense. The Clinical Pharmacogenetics Implementation Consortium (CPIC) an expert group that publishes guidelines for using genetic data in prescribing recommends testing before restarting simvastatin in anyone with prior muscle symptoms. Some doctors also test people before prescribing high-dose simvastatin, especially if they’re older, have kidney issues, or take other drugs that interact with statins. But routine testing for everyone starting statins? Not yet. The evidence isn’t strong enough to prove it saves lives or cuts heart attacks in the general population. Still, for people who’ve already struggled, it’s a game-changer. A 2021 Mayo Clinic survey found that 78% of patients with prior statin intolerance were able to restart statin therapy successfully after genetic testing guided their choice. One woman, 54, had to stop simvastatin after severe leg cramps. Her test showed CC genotype. She switched to pravastatin. Her LDL dropped from 168 to 92. No more pain. She’s been on it for 18 months.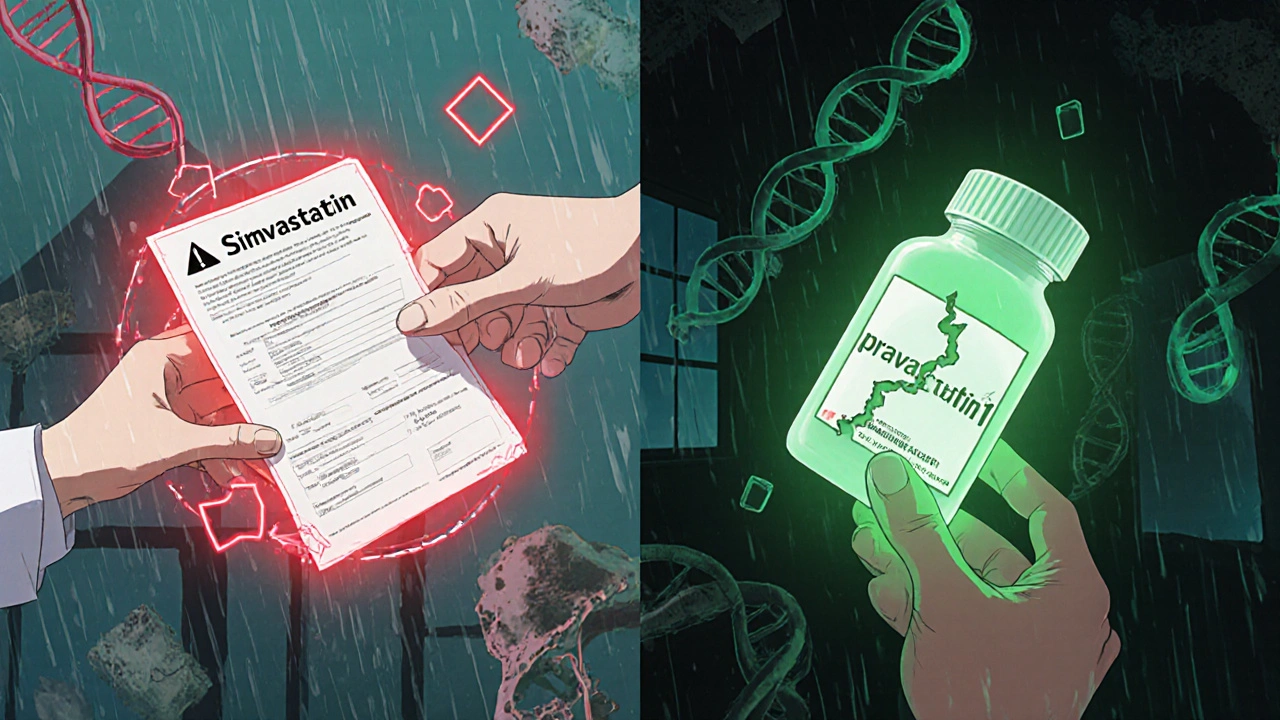
What the Test Actually Involves
Getting tested is simple. You spit into a tube or get a cheek swab. No needles. No fasting. The sample goes to a lab-companies like Mayo Clinic Laboratories a leading provider of clinical pharmacogenomic testing, ARUP Laboratories a national reference lab offering PGx panels, or Color Genomics a direct-to-consumer genetic testing company offering pharmacogenomic panels. Results come back in about a week. The report will tell you your SLCO1B1 genotype: TT, TC, or CC. If you’re CC, you’ll be advised to avoid simvastatin 80mg entirely. If you’re TC, lower doses of simvastatin (under 40mg) may be okay, but switching to pravastatin or rosuvastatin is safer. The report usually includes dosing recommendations from CPIC guidelines. Some labs bundle this with tests for other genes like CYP2D6 a liver enzyme that metabolizes some statins and other drugs and ABCB1 a gene that affects how statins are pumped out of cells, which may add more context. But SLCO1B1 is the only one with strong, clear guidelines.The Catch: It’s Not Perfect
Here’s the reality check: SLCO1B1 explains only about 6% of all statin muscle symptoms. That means most people who get muscle pain still don’t have this gene variant. Other genes, like GATM a gene linked to creatine metabolism and muscle energy and CACNA1S a gene involved in muscle contraction, are being studied, but nothing else is ready for clinical use yet. And here’s the bigger problem: even when you get the right statin, some people still get muscle pain. Why? We don’t fully know. Maybe it’s vitamin D deficiency. Maybe it’s thyroid issues. Maybe it’s just the placebo effect of expecting pain. But that doesn’t make the pain any less real. A 2020 Harvard study gave SLCO1B1 results to doctors treating patients with prior statin intolerance. Guess what? It didn’t improve adherence or reduce symptoms. Patients still quit. Why? Because doctors didn’t know what to do with the results. Many primary care physicians say they feel unprepared to interpret them without decision tools built into their electronic records.
Insurance, Cost, and Access
The test costs between $150 and $400 out of pocket. Insurance coverage is patchy. Only about 28% of private insurers covered it in 2022. Medicare rarely pays unless it’s part of a research program. That’s a big barrier. Some companies offer testing as part of broader wellness panels. But be careful: direct-to-consumer tests like 23andMe don’t give you clinical-grade results or interpretation. You need a test ordered by a doctor or through a certified lab with clear guidance.What’s Next?
Researchers are working on polygenic risk scores-combining SLCO1B1 with 10-15 other small-effect genes to better predict who’ll have trouble. Early results show they can improve prediction from 58% accuracy to 67%. That’s promising, but not ready for clinics yet. Meanwhile, hospitals like those in the Statin Pharmacogenomics Implementation Consortium a multi-center effort to standardize genetic testing for statin use are rolling out EHR alerts. If a doctor tries to prescribe simvastatin 80mg to someone with a CC genotype, the system pops up a warning. That’s how change happens-at the point of care.What You Can Do Today
If you’ve quit statins because of muscle pain:- Ask your doctor if SLCO1B1 testing is right for you.
- Don’t assume you’re "statin intolerant"-you might just be intolerant to the wrong one.
- Pravastatin and rosuvastatin are your best bets if you have the risky gene.
- If your doctor says no, ask for a referral to a cardiologist or pharmacogenomics clinic.
- Check PharmGKB.org for free, updated gene-drug guidelines.
Is genetic testing for statin tolerance worth it?
It’s worth it if you’ve had muscle pain on statins before. For people who stopped statins due to muscle symptoms, testing can identify whether SLCO1B1 is the cause-and point you toward safer alternatives like pravastatin or rosuvastatin. Studies show 78% of these patients can successfully restart statin therapy after testing. For people without prior side effects, testing isn’t routinely recommended yet because it hasn’t been proven to improve heart outcomes in the general population.
Does every statin cause the same muscle problems?
No. Simvastatin has the strongest link to SLCO1B1-related muscle issues, especially at high doses. Atorvastatin and rosuvastatin are much less affected by this gene variant. Pravastatin and fluvastatin barely use the transporter at all, making them safer choices for people with the risky gene. Your risk depends on both the drug and your genes.
Can I get tested without seeing a doctor?
Yes, you can order direct-to-consumer tests from companies like Color or 23andMe. But most of these don’t provide clinical-grade results or interpretation for statins. You need a test ordered through a healthcare provider or certified lab like Mayo Clinic or ARUP, which includes a clear report with dosing recommendations based on CPIC guidelines.
Will my insurance cover this test?
It depends. Only about 28% of private insurers covered SLCO1B1 testing in 2022. Medicare rarely pays unless it’s part of a research study. If you’re being tested after experiencing side effects, your doctor may be able to argue medical necessity. Out-of-pocket costs range from $150 to $400.
What if I test positive but still get muscle pain?
SLCO1B1 explains only about 6% of statin muscle symptoms. If you still have pain after switching to a safer statin, other factors may be involved-like low vitamin D, thyroid problems, overexertion, or interactions with other medications. Talk to your doctor about checking these. You might need to adjust your dose, timing, or try a non-statin option like ezetimibe or PCSK9 inhibitors.




giri pranata
October 29, 2025 at 15:38
Wow, this is life-changing info! I’ve been avoiding statins for years because of muscle pain, but never thought it could be my genes. Just got my SLCO1B1 results back-TC genotype. My doc switched me to pravastatin last month and I haven’t felt this good in years. No cramps, no fear. Seriously, if you’ve quit statins, get tested. It’s not magic, it’s science. 🙌