Caffeine & Medication Interaction Checker
Check Your Medication Interaction
Enter your current medication and caffeine intake to get personalized safety guidance
Enter your medication and caffeine intake to see interaction results
Most people drink coffee without thinking twice. But if you’re on medication, that morning cup could be doing more than just waking you up-it might be making your drugs less effective, or even dangerous. You might not realize it, but caffeine doesn’t just buzz through your system. It plays hardball with your medications, changing how they’re absorbed, broken down, or how they work in your body. And the consequences aren’t theoretical. People end up in emergency rooms because of this. Thousands of them, every year.
Why Caffeine Interferes With Your Meds
Caffeine isn’t just a stimulant. It’s a chemical that talks directly to your liver. Specifically, it messes with an enzyme called CYP1A2, which is responsible for breaking down about 1 in 10 prescription drugs. When caffeine blocks this enzyme, your body can’t clear certain medications the way it should. That means those drugs stick around longer, building up to unsafe levels. Other times, caffeine blocks the drug’s action entirely-like when it stops heart medications from working during stress tests.
It’s not just coffee. Tea, energy drinks, chocolate, and even some painkillers contain caffeine. Decaf? Still has 2-15 mg per cup. For people on sensitive meds, that’s enough to cause problems.
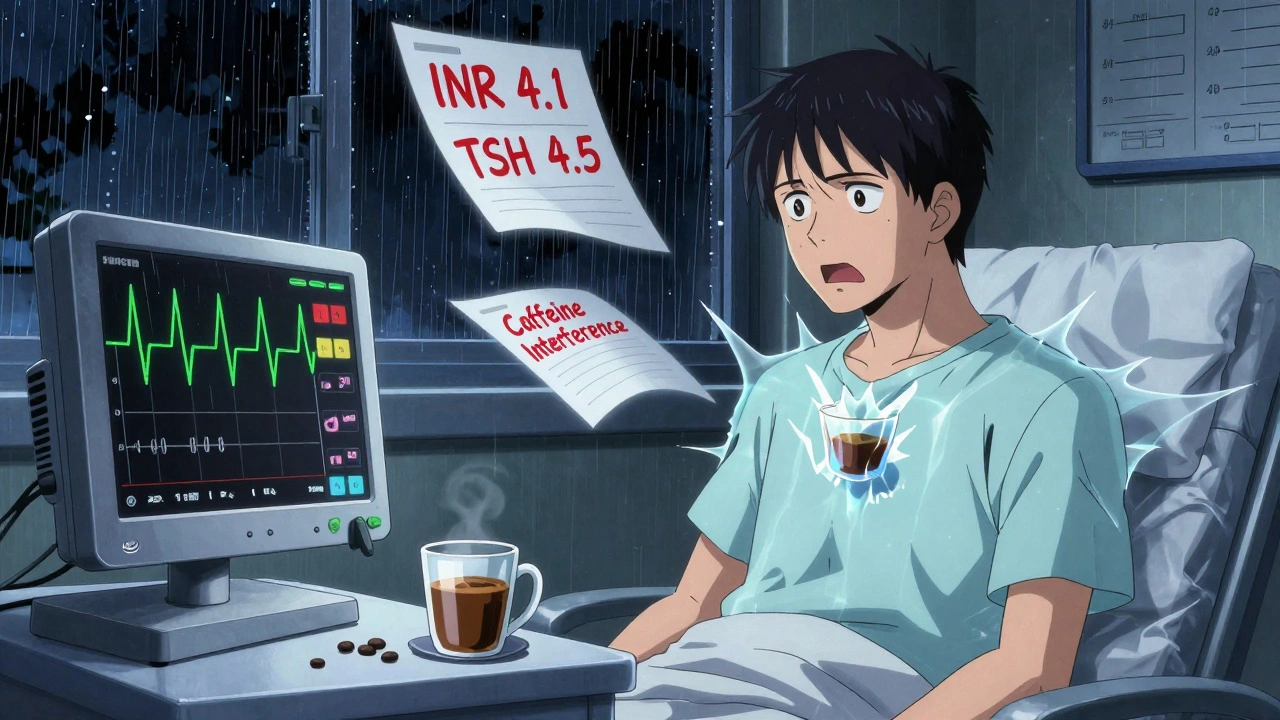
Warfarin and Blood Thinners: The Silent Risk
If you’re taking warfarin (Coumadin), your blood thinning levels are already a tightrope walk. Caffeine can throw you off balance. Studies show that drinking coffee with warfarin can raise your INR-your blood’s clotting time-by 15-25% within just 24 hours. That means your blood takes longer to clot, increasing your risk of internal bleeding. One patient in Sydney reported bleeding gums after switching from tea to espresso. Her INR jumped from 2.3 to 4.1 in three days.
The American Heart Association recommends limiting caffeine to 200 mg per day (about two cups of coffee) if you’re on warfarin. But even that’s not safe if your intake swings around. Consistency matters. If you usually drink two cups and suddenly switch to one, your INR could drop. If you go from one to four, your risk spikes. The key? Stick to the same amount every day-and tell your doctor what you drink.
Thyroid Medication: The 60-Minute Rule
Levothyroxine (Synthroid, Levoxyl) is one of the most commonly prescribed drugs in the world. And it’s one of the most sensitive to caffeine. A 2017 study of 98 patients showed coffee reduced levothyroxine absorption by 25-57%. That’s not a small drop. It means your thyroid levels stay high, your TSH stays elevated, and your fatigue, weight gain, and brain fog don’t improve.
One Reddit user shared: “My TSH was 4.5 after years of being stable at 1.8. I didn’t change my dose-I just started drinking coffee right after my pill. I waited 60 minutes after taking it, and my levels went back to normal.”
The Endocrine Society’s official advice? Wait at least 30-60 minutes after taking your thyroid pill before drinking coffee or eating breakfast. Some doctors recommend waiting up to 90 minutes for maximum effect. Don’t skip this step. It’s not a suggestion-it’s a medical necessity.
Heart Medications: Don’t Risk a Failed Stress Test
Adenosine and dipyridamole are used during cardiac stress tests to simulate exercise and check for blocked arteries. But caffeine blocks the exact receptors these drugs need to work. One cup of coffee can reduce their effectiveness by up to 50%.
The American College of Cardiology’s 2023 guidelines are clear: no caffeine for 24 hours before a stress test. Not one sip. Not one chocolate bar. Not even decaf.
On HealthTap, a patient wrote: “I had one cup of coffee before my test. The results were inconclusive. I had to reschedule-and pay another $800.”
Even if you’re not getting tested, caffeine can interfere with beta-blockers and calcium channel blockers like verapamil. Mayo Clinic notes that caffeine can raise diastolic blood pressure by 8-12 mmHg for several hours after consumption. For someone already managing hypertension, that’s enough to undo the benefits of their medication.
Antidepressants and Psychiatric Drugs: Anxiety on Steroids
SSRIs like fluvoxamine (Luvox) and escitalopram (Lexapro) are metabolized by CYP1A2. Caffeine slows that process, causing drug levels to rise. That sounds good-until you realize it can trigger severe anxiety, insomnia, heart palpitations, or even serotonin syndrome.
Harvard Health reports that fluvoxamine’s absorption drops by 33% when taken with coffee. But for tricyclic antidepressants like amitriptyline, the opposite happens: caffeine increases blood levels by 20-40%, raising the risk of dizziness, dry mouth, confusion, and irregular heartbeat.
Patients on Drugs.com report that 68% experienced worse anxiety when combining caffeine with psychiatric meds. One user wrote: “I took my Lexapro with coffee and felt like I was having a panic attack at 9 a.m. I thought I was losing my mind. Turns out, the coffee was the trigger.”
Dr. Robert H. Shmerling of Harvard Health puts it bluntly: “Drinking coffee-especially in large amounts-can affect how your body processes these drugs.”
Seizure Medications: A Dangerous Combo
If you have epilepsy or are on drugs like carbamazepine, phenytoin, or valproate, caffeine can be a trigger. It lowers the seizure threshold. Research in Epilepsy & Behavior found that patients who consumed caffeine regularly had 18-35% more seizures than those who avoided it.
It’s not just about the amount-it’s about consistency. Suddenly cutting back on caffeine after years of daily use can also trigger seizures. If you’re on these meds, don’t quit coffee cold turkey. Talk to your neurologist about tapering.
Stimulants and ADHD Meds: The Jittery Trap
Adderall, Ritalin, and other stimulants for ADHD already speed up your heart and nervous system. Add caffeine to that, and you’re stacking fuel on fire.
University Hospitals’ 2025 update found that combining caffeine with amphetamines or pseudoephedrine can spike heart rate by 20-35 beats per minute and raise systolic blood pressure by 15-25 mmHg within 45 minutes. One patient on PatientsLikeMe said: “I took my Adderall with coffee and couldn’t sleep for 12 hours. My heart felt like it was in my throat.”
For diabetics, this combo is even riskier. Pseudoephedrine with caffeine can raise blood sugar by 15-25 mg/dL and increase body temperature by 0.5-1.0°C. That’s a double threat-worsening both diabetes control and cardiovascular strain.
What You Should Do
Here’s what works in real life:
- Know your meds. Check if your prescription has a caffeine warning. If you’re unsure, ask your pharmacist.
- Separate your coffee and your pills. For thyroid meds: wait 60 minutes. For most others: wait at least one hour before or two hours after caffeine.
- Be consistent. If you drink coffee, drink the same amount every day. Don’t skip days or double up.
- Watch for hidden caffeine. Energy drinks, soda, chocolate, and even some headache pills contain caffeine. Read labels.
- Track your symptoms. Did your anxiety get worse? Did your blood pressure spike? Did your thyroid levels change? Note it down and bring it to your doctor.
When to Seek Help
Some reactions need emergency care. If you experience any of these after combining caffeine and medication, call 000 or go to the nearest ER:
- Heart rate over 120 bpm
- Systolic blood pressure above 180 mmHg
- Difficulty breathing
- Confusion, vision changes, or loss of coordination
- Twitching, rigid muscles, or shaking
- Seizures or altered mental state
- Worsening depression or suicidal thoughts
These aren’t rare. They happen. And they’re preventable.
The Bigger Picture
Over 150 million Americans are at risk of caffeine-medication interactions. In Australia, the numbers are similar. These interactions cost the healthcare system over $1.2 billion a year in avoidable ER visits, lab tests, and hospitalizations.
Major hospitals now screen for caffeine use in electronic health records. Pharmacists are trained to ask: “Do you drink coffee or energy drinks?” But you can’t rely on them to catch everything. You need to speak up.
It’s not about giving up coffee. It’s about taking control. Your meds are working hard to keep you healthy. Don’t let caffeine sabotage them.



Stacy Foster
December 12, 2025 at 08:40
Of course the government doesn't want you to know this. Big Pharma and Big Coffee are in bed together. They've been suppressing studies since the 90s. I've seen the leaked memos - they call it 'The Caffeine Cover-Up.' You think your doctor knows? Nah. They get paid to keep you docile. That 60-minute rule? A distraction. You need to wait 90 minutes, use distilled water, and take your meds in a Faraday cage. I'm not even kidding.