COVID-19 Treatment Decision Tool
Personalized Treatment Recommendations
This tool helps you understand which COVID-19 treatment might be most appropriate for your situation based on key factors like your health status, symptoms, and treatment availability.
Quick Takeaways
- Movfor (Molnupiravir) lowers hospitalisation risk by about 30% when started early.
- Paxlovid consistently shows 89% risk reduction but requires a boosting pill and has drug‑interaction limits.
- Remdesivir is given intravenously, useful for hospitalised patients, but less convenient for out‑of‑hospital use.
- Monoclonal antibodies (e.g., sotrovimab) work well against earlier variants but lose potency against newer Omicron sub‑lineages.
- Cost, availability and patient comorbidities often decide which option is best.
What is Movfor (Molnupiravir)?
When you first see the name Movfor is the brand name for Molnupiravir, an oral antiviral approved for treating mild‑to‑moderate COVID‑19 in adults at risk of severe disease. It was developed by Merck & Ridgeback and received emergency use authorisation in many countries in 2022.
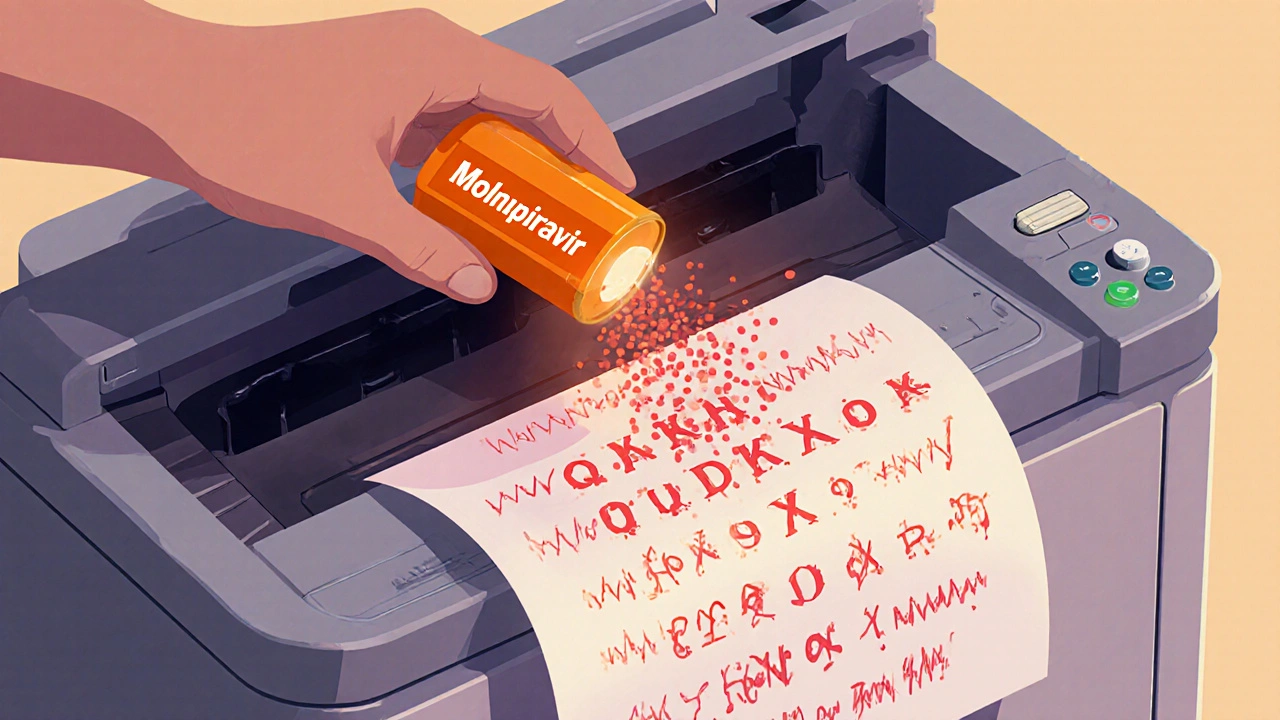
The drug works by introducing copying errors into the virus’s RNA, a strategy called "error‑inducing mutagenesis." In plain English, it tricks the virus into making a faulty genome, which stops it from replicating effectively.
How Does Molnupiravir Work? (The Mechanism in Everyday Terms)
Think of the coronavirus as a copy‑machine. Every time it makes a new copy of its genetic code, there’s a chance for a typo. Molnupiravir hands the virus a faulty ink cartridge, causing it to insert a lot more typos than normal. After enough mistakes pile up, the virus can’t function properly and the infection fizzles out.
The drug is taken as 800mg twice a day for five days, and it works best when started within five days of symptom onset. That timing window is critical - the earlier you stop the copy‑machine, the less virus there is to cause trouble.
The Main Alternatives on the Market
Before we stack them side by side, let’s meet the other players you’ll hear about.
Paxlovid is a combo of nirmatrelvir (the antiviral) and ritonavir (a booster that slows drug breakdown). It’s the current front‑runner for outpatient COVID‑19 treatment, showing 89% reduction in hospitalisation in the EPIC‑HR trial.
Remdesivir is an intravenous nucleotide analogue that blocks the viral polymerase. It’s the only COVID‑19 drug that earned full FDA approval for hospitalised patients.
Sotrovimab is a monoclonal antibody that binds to a conserved region of the spike protein, neutralising the virus. It’s administered as a single IV infusion.
Fluvoxamine is an SSRI that has off‑label anti‑inflammatory effects in COVID‑19, likely via sigma‑1 receptor activation. It’s cheap and oral, but evidence is mixed.
Other noteworthy mentions include Veklury (the brand name for Remdesivir) and the regulatory bodies that approve them - the FDA and the European Medicines Agency (EMA).
Head‑to‑Head Efficacy: Numbers That Matter
When you compare antivirals, the key metric most people ask for is “how much does this cut my chance of ending up in the hospital?” Below is a snapshot of the latest data from large‑scale trials and real‑world studies up to September2025.
| Drug | Mechanism | Hospitalisation Risk Reduction | Typical Administration | Common Side Effects | Key Contra‑indications |
|---|---|---|---|---|---|
| Movfor (Molnupiravir) | Error‑inducing mutagenesis | ~30% (placebo‑controlled MOVe‑OUT trial) | 800mg PO BID ×5days | Diarrhoea, nausea, dizziness | Pregnancy, severe renal impairment |
| Paxlovid (nirmatrelvir/ritonavir) | Protease inhibition + boosting | ~89% (EPIC‑HR trial) | 300mg PO BID + 100mg ritonavir BID ×5days | Altered taste, hypertension, diarrhea | Strong CYP3A4 inhibitors, severe liver disease |
| Remdesivir (Veklury) | Polymerase chain termination (IV) | ~87% when given within 7days (ACTT‑1) | 200mg IV day1 then 100mg daily ×4days | Elevated liver enzymes, renal dysfunction | eGFR<30ml/min, hypersensitivity |
| Sotrovimab | Spike‑protein neutralising antibody | ~85% (COMET‑ICE) against pre‑Omicron strains | 500mg IV single infusion | Infusion‑site reactions, rash | Known hypersensitivity to monoclonals |
| Fluvoxamine | Sigma‑1 receptor agonist (anti‑inflammatory) | ~25% (TOGETHER trial) - mixed real‑world data | 100mg PO BID ×10days | Nausea, insomnia, sweating | Concomitant MAO‑I use, severe hepatic disease |
Notice how Paxlovid leads the pack, but it also brings a complex drug‑interaction profile because of ritonavir. Molnupiravir sits in the middle - modest efficacy, but the simplest regimen and few interactions.
Safety and Side‑Effect Profile: What to Watch For
Every medication has a downside, so let’s break it down in everyday language.
- Movfor: Mostly mild GI upset. The biggest red flag is use in pregnancy - animal studies showed potential fetal harm, so it’s contraindicated.
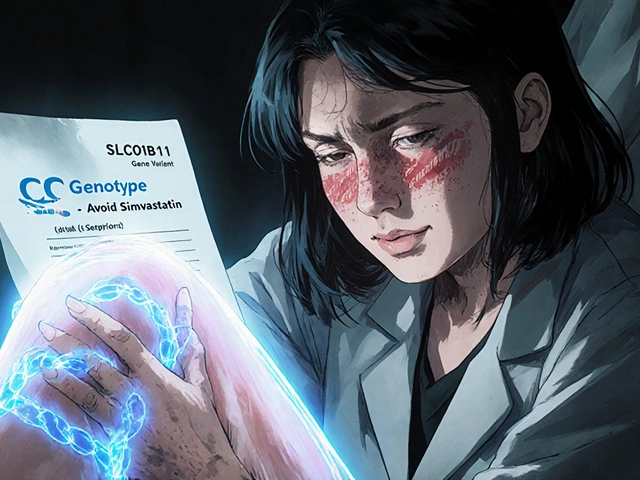
- Paxlovid: The ritonavir booster can crank up levels of many other drugs (statins, certain anti‑arrhythmics). Always run a quick medication‑review before prescribing.
- Remdesivir: Needs IV access, and kidney function should be checked because the formulation contains a solubilising agent that can accumulate.
- Sotrovimab: Infusion reactions are rare but can happen. Because it’s a protein, patients with severe immunodeficiency may not benefit as much.
- Fluvoxamine: As an SSRI, it can cause serotonin syndrome if mixed with other serotonergic meds. Also watch for sleep disturbances.
In practice, the simplest safety check for Molnupiravir is a pregnancy test for women of childbearing potential and a quick glance at renal labs.

Practical Decision Guide: When to Choose Which Drug
Imagine you’re a primary‑care doctor with a 45‑year‑old patient who just tested positive, has hypertension, and takes atorvastatin. Here’s a quick mental flow‑chart:
- If the patient can start treatment within 5days and has no major drug‑interaction concerns, Paxlovid is the first choice because of its superior efficacy.
- If the patient is on multiple CYP3A4‑dependent drugs (like certain anti‑arrhythmics) that you can’t safely pause, consider Movfor - it doesn’t need boosting.
- If the patient is already hospitalised or has severe renal impairment, Remdesivir (IV) becomes the go‑to.
- If the circulating variant is known to be susceptible and the patient can get an infusion quickly, Sotrovimab is an option, especially for immunocompromised folks.
- If cost is a major barrier and the patient is low‑risk, Fluvoxamine could be a stop‑gap, but discuss the limited evidence.
This algorithm keeps the focus on three things: timing, comorbidities, and drug interactions.
Cost, Access, and Real‑World Availability (2025 Snapshot)
Pricing can tip the scales dramatically, especially in low‑income settings.
- Movfor: RoughlyAU$250 for a 5‑day pack in Australia; insurance often covers it for high‑risk patients.
- Paxlovid: AboutAU$400 for the full course, but most government programs subsidise it for people over 65 or with chronic illness.
- Remdesivir: Hospital cost runs >AU$1,200 per treatment cycle, reflecting IV administration.
- Sotrovimab: AroundAU$1,500 per dose; availability limited to infusion centres.
- Fluvoxamine: Generic SSRI price is
Supply chains have stabilised after the 2023 shortages, but local pharmacy stock can still vary. Always check the national therapeutic goods register for the latest stock alerts.
Quick Checklist for Clinicians
- Confirm COVID‑19 positive test and symptom onset ≤5days.
- Assess patient risk factors (age≥60, comorbidities, immunosuppression).
- Review current medications for CYP3A4 interactions.
- Pregnancy test for women of childbearing potential before prescribing Movfor.
- Choose:
- Paxlovid for highest efficacy if no interaction issues.
- Movfor when interactions or contraindications to Paxlovid exist.
- Remdesivir for hospitalized or severe renal impairment.
- Sotrovimab for rapid infusion eligibility and variant‑susceptibility.
- Fluvoxamine only as low‑cost fallback with patient consent.
- Document prescription, provide patient education sheet, and schedule follow‑up call at day3.
Frequently Asked Questions
Can I take Movfor if I’m already on a blood‑thinner?
Yes, Molnupiravir does not affect clotting pathways, so it’s safe alongside anticoagulants like warfarin or apixaban. Just monitor your usual blood‑test schedule.
How quickly does Movfor start working?
Viral load typically drops within 48hours of the first dose, assuming treatment begins early. Early viral suppression translates to fewer symptoms and lower hospital risk.
Is there any risk of the virus becoming resistant to Molnupiravir?
The error‑inducing mechanism makes resistance unlikely because the drug forces the virus to accumulate many mutations at once, which generally renders it non‑viable.
Can I use Movfor for prophylaxis after exposure?
Currently, Molnupiravir is only approved for treatment, not prevention. Post‑exposure prophylaxis studies are still ongoing.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s less than 6hours before the next scheduled dose. In that case, skip the missed one and continue the regular schedule - don’t double‑dose.
By matching the right drug to the right patient, you can keep COVID‑19 from landing anyone in the hospital. Whether you reach for the high‑powered Paxlovid, the low‑interaction Movfor, or another option, the key is early testing, quick prescribing, and a clear safety check.



Cassidy Strong
October 15, 2025 at 05:46
Molnupiravir, marketed under the brand name Movfor, operates by introducing copying errors into the viral RNA; this mechanism, known as error‑inducing mutagenesis, effectively hampers viral replication.
Its oral administration-800 mg taken twice daily for five days-offers a practical advantage over intravenous alternatives such as Remdesivir.
Clinical data from the MOVe‑OUT trial indicate approximately a 30 % reduction in hospitalisation risk when therapy commences within five days of symptom onset.
In contrast, Paxlovid (nirmatrelvir/ritonavir) demonstrates a markedly higher efficacy, around an 89 % reduction, yet its use is constrained by significant drug‑interaction potential.
Remdesivir, while achieving up to an 87 % risk reduction when administered early, requires infusion in a clinical setting, limiting its utility for out‑patient treatment.
Sotrovimab, a monoclonal antibody, retains potency against earlier SARS‑CoV‑2 variants but has lost effectiveness against recent Omicron sub‑lineages, thereby reducing its relevance in current practice.
The cost dimension further differentiates these therapies: Molnupiravir’s pricing is generally lower than that of monoclonal antibodies, yet higher than generic options like fluvoxamine.
Renal and hepatic considerations also influence selection; severe kidney disease may preclude Molnupiravir due to renal clearance concerns, while significant liver impairment necessitates dose adjustments for Paxlovid.
Pregnancy presents an additional contraindication for Molnupiravir, underscoring the need for alternative options for this demographic.
From a public‑health perspective, the availability of an oral antiviral that does not require boosting agents simplifies distribution in resource‑limited settings.
However, the modest efficacy relative to Paxlovid should temper expectations; clinicians must weigh the trade‑off between convenience and therapeutic potency.
Real‑world studies up to September 2025 suggest that early initiation-ideally within the first three days of symptom onset-optimises outcomes for all oral antivirals.
Adherence remains a critical factor; the twice‑daily dosing schedule of Molnupiravir may pose challenges for some patients compared to the single‑dose regimen of certain monoclonal antibodies.
Pharmacovigilance reports have highlighted gastrointestinal side effects-diarrhoea, nausea, and occasional dizziness-as the most common adverse events associated with Molnupiravir.
In contrast, Paxlovid’s side‑effect profile includes altered taste and hypertension, which may be problematic for individuals with pre‑existing cardiovascular disease.
Ultimately, the selection of an appropriate COVID‑19 outpatient therapy must integrate efficacy data, patient comorbidities, drug‑interaction risk, and logistical considerations to achieve the best clinical outcome.