Serotonin Syndrome Risk Calculator
Your Medication Choices
Additional Risk Factors
Please select your medications to see your risk assessment.
Combining SSRIs and opioids might seem harmless if you’re just following your doctor’s orders. But for thousands of people, this everyday combination can trigger something dangerous - serotonin syndrome. It doesn’t happen often, but when it does, it can turn deadly in hours. You might feel fine one minute, then suddenly your body starts shaking, your heart races, and you can’t stop sweating. It’s not anxiety. It’s not a fever. It’s serotonin syndrome - and it’s preventable if you know what to look for.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t an allergy. It’s a chemical overload. Your brain and nerves rely on serotonin to regulate mood, sleep, and pain. SSRIs like sertraline, fluoxetine, and escitalopram work by keeping more serotonin active in your system. Opioids like tramadol, methadone, and even codeine can do the same thing - not by boosting serotonin directly, but by blocking its cleanup. When both are taken together, serotonin builds up faster than your body can clear it. The result? Overstimulated nerves, runaway muscle contractions, and a body that can’t regulate its own temperature.The symptoms start small. A sudden shiver you can’t stop. A twitch in your leg. A rapid heartbeat. Then it escalates: high fever, stiff muscles, confusion, seizures. In severe cases, body temperature can hit 41°C (106°F). Without quick treatment, organ failure or death can follow. Emergency rooms see this more often than you think - and many cases are misdiagnosed as strokes, infections, or drug withdrawal.
Not All Opioids Are Created Equal
If you’re on an SSRI and need pain relief, not all opioids carry the same risk. Some are low-risk. Others are ticking time bombs.High-risk opioids: Tramadol, methadone, and pethidine (meperidine). These don’t just relieve pain - they directly block serotonin reuptake. Tramadol is especially dangerous. Studies show it’s 30 times more likely to cause serotonin syndrome than morphine. In fact, nearly 4 out of 10 serotonin syndrome cases linked to opioids involve tramadol. Even at normal doses, it can trigger symptoms when combined with SSRIs.
Lower-risk opioids: Morphine, oxycodone, hydromorphone, and buprenorphine. These work mainly on opioid receptors without interfering much with serotonin. They’re safer choices if you’re already on an SSRI. Fentanyl is tricky - lab tests say it shouldn’t cause issues, but real-world reports show over 120 cases of serotonin syndrome linked to it. Why? It might interact with serotonin receptors in ways we don’t fully understand yet.
And yes, even codeine - often thought of as safe - has caused serotonin syndrome in people taking SSRIs. That case report from 2018? It changed the rules. No opioid is completely risk-free when paired with an SSRI.
Some SSRIs Are Riskier Than Others
Fluoxetine (Prozac) is the worst offender among SSRIs - not because it’s stronger, but because it sticks around. Its active metabolite, norfluoxetine, can stay in your system for up to 16 days after you stop taking it. That means even if you quit Prozac a week before starting tramadol, you’re still at risk. Sertraline and citalopram clear faster - around 26 hours for sertraline - so the window for interaction is smaller.SNRIs like venlafaxine (Effexor) are even riskier than SSRIs because they also block norepinephrine reuptake. Add one of those to tramadol, and you’re stacking two powerful serotonin boosters. MAOIs - older antidepressants like phenelzine - are the most dangerous of all. Combining them with any opioid can be fatal. That’s why doctors require a 14-day washout period before switching from an MAOI to another antidepressant. For fluoxetine? You need five weeks.

Who’s Most at Risk?
It’s not just about the drugs. Your body matters too.Older adults are at higher risk. People over 65 take an average of 31% more medications than younger adults. More pills = more chances for bad interactions. People with kidney or liver disease are also vulnerable. If your body can’t break down drugs properly, even normal doses can become toxic.
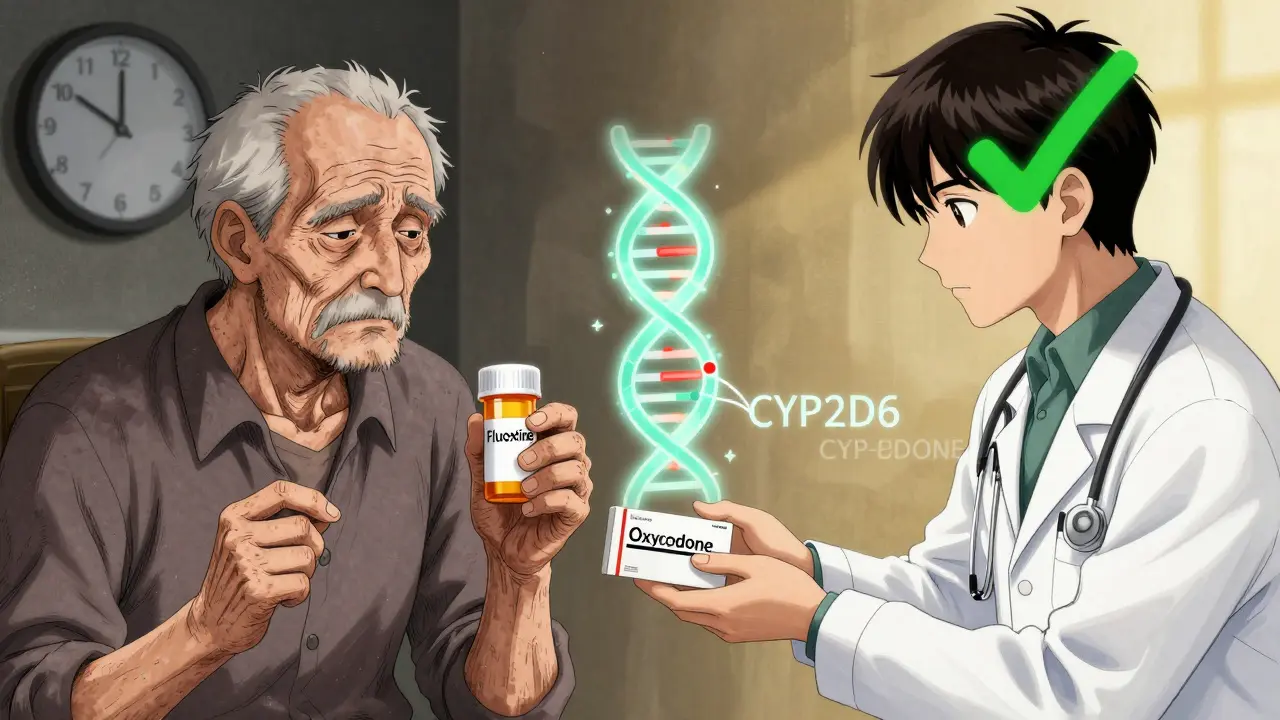
Genetics play a role too. About 7% of people have a genetic variation that makes them poor metabolizers of the CYP2D6 enzyme - the same enzyme that breaks down tramadol. If you’re one of them, tramadol builds up faster in your blood. Studies show these people are over three times more likely to develop serotonin syndrome. Most doctors don’t test for this - but if you’ve had a bad reaction to pain meds before, it’s worth asking.
How to Prevent It
Prevention isn’t about avoiding all opioids. It’s about making smarter choices.- Avoid tramadol, methadone, and pethidine if you’re on an SSRI or SNRI. Ask for morphine, oxycodone, or hydromorphone instead.
- Never start a new opioid while on an SSRI without talking to your doctor. If you’re switching antidepressants, wait at least two weeks - five weeks if you were on fluoxetine.
- Start low, go slow. If an opioid is absolutely necessary, your doctor should begin with half the usual dose and watch you closely for 72 hours.
- Check your EHR. Many hospitals now have systems that flag dangerous combinations. If your pharmacy or doctor doesn’t warn you, ask why.
One hospital system in the U.S. cut dangerous tramadol-SSRI prescriptions by 87% just by adding a hard stop in their electronic record system. That’s not magic - it’s basic safety design.
What to Do If Symptoms Start
If you or someone you know starts showing signs - shivering, muscle spasms, fast heartbeat, confusion, high fever - stop the medications immediately. Don’t wait. Call emergency services. Tell them you suspect serotonin syndrome.At the hospital, treatment is straightforward: stop the drugs, give benzodiazepines to calm the nervous system, cool the body if overheated, and give cyproheptadine - a serotonin blocker - if it’s severe. Most people recover within 24 to 72 hours if treated early. Delayed treatment? That’s when things turn fatal.
Don’t assume it’s just a bad reaction to pain meds. If you’ve been on an SSRI and suddenly feel off after starting an opioid, it’s not ‘just stress.’ It’s serotonin syndrome - and it’s treatable if caught fast.
What’s Changing in 2026?
Regulators are finally catching up. The FDA now requires all opioid medication guides to include serotonin syndrome warnings. The European Medicines Agency updated tramadol labels in 2021. In Australia, the Therapeutic Goods Administration now lists tramadol-SSRI combinations as a ‘high-priority interaction’ in clinical guidelines.Next up: smarter tech. Epic Systems - the biggest electronic health record provider - is rolling out new tools in 2024 that will analyze your genes, your meds, and your kidney function to predict your personal risk. For the first time, your doctor might see a pop-up saying: ‘High risk: CYP2D6 poor metabolizer + tramadol + sertraline. Consider oxycodone instead.’
Meanwhile, the NIH is funding $2.4 million to find early biomarkers - chemical signals in blood that appear before symptoms show up. Imagine a simple blood test that warns you before you even feel sick.
Final Word
You’re not being paranoid if you’re worried about your meds. Serotonin syndrome is rare - but it’s real, it’s dangerous, and it’s avoidable. If you’re on an SSRI and your doctor suggests tramadol for pain, say no. Ask for an alternative. If you’re already on both and feel strange - don’t ignore it. Write down your symptoms. Call your doctor. If you can’t reach them, go to the ER.Medications are powerful tools. But they’re not harmless. The safest choice isn’t always the one that’s easiest - it’s the one that keeps you alive.
Can you get serotonin syndrome from just one drug?
Rarely. Serotonin syndrome almost always happens when two or more serotonergic drugs are combined. Taking a high dose of an SSRI alone can cause it, but it’s uncommon. Most cases involve mixing antidepressants with opioids, certain migraine meds, or herbal supplements like St. John’s Wort.
Is tramadol the only opioid I should worry about?
No, but it’s the most common culprit. Methadone and pethidine are also high-risk. Even fentanyl and codeine have been linked to serotonin syndrome in real cases, even though lab tests suggest they shouldn’t cause it. Don’t assume any opioid is safe if you’re on an SSRI - always check with your doctor.
How long should I wait after stopping an SSRI before taking an opioid?
It depends on the SSRI. For sertraline or citalopram, wait at least 7 days. For fluoxetine (Prozac), wait 5 weeks because it stays in your system so long. Never guess - ask your pharmacist or doctor for the exact timeline based on your specific medication.
Can I use over-the-counter painkillers like ibuprofen instead?
Yes, for mild to moderate pain. NSAIDs like ibuprofen or naproxen don’t affect serotonin and are generally safe with SSRIs. But if you have kidney issues, stomach ulcers, or heart disease, talk to your doctor first. They’re safer than tramadol, but not risk-free.
What should I do if my doctor prescribes tramadol with my SSRI?
Ask why. Say: ‘I’ve read that combining these can cause serotonin syndrome. Are there safer alternatives like oxycodone or morphine?’ Most doctors aren’t aware of the full risk - but if you bring up the data, they’ll reconsider. Your life is worth pushing for.





Katie and Nathan Milburn
January 30, 2026 at 23:30
Thank you for this meticulously researched piece. As a clinical pharmacist with over two decades in geriatric care, I’ve seen too many patients admitted for serotonin syndrome after being prescribed tramadol for ‘mild’ back pain while on sertraline. The real tragedy isn’t the syndrome itself-it’s how often it’s dismissed as ‘anxiety’ or ‘flu.’ Documentation and patient education are the two most underused tools in prevention.