EHR Allergy Records: How Digital Systems Track and Improve Allergy Safety
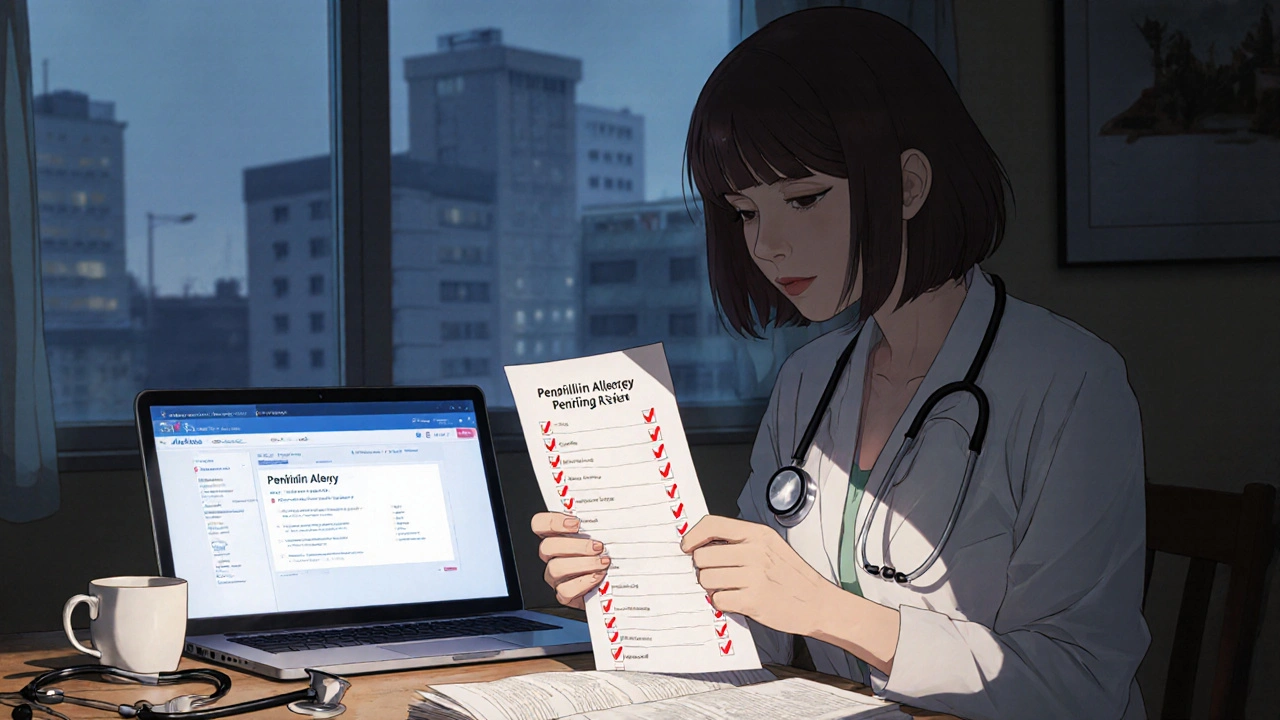
When your doctor pulls up your EHR allergy records, digital logs of your known allergies and adverse reactions stored in an electronic health record system. Also known as allergy alerts in EHRs, these records are meant to stop a life-threatening reaction before it starts. But they don’t always work right. A patient with a documented penicillin allergy might still get prescribed it—not because the doctor ignored the warning, but because the EHR flagged it as "possible" instead of "confirmed," or the alert got buried under 20 other pop-ups. This isn’t rare. Studies show over 30% of allergy alerts in EHRs are clinically irrelevant, and many real allergies go unrecorded because patients forget to mention them or providers don’t document them clearly.
That’s why electronic health records, digital versions of a patient’s medical history used by clinics and hospitals to manage care. Also known as EMRs, they are the backbone of modern prescribing need to be smarter. An EHR allergy record isn’t just a note—it’s a live safety tool. It should link to your medication history, flag interactions with drugs like OTC antihistamine choices you might pick on your own, and warn about cross-reactivity (like how sulfa allergies sometimes mean you can’t take certain diuretics). But most systems still treat allergies as static text, not dynamic data. They don’t know if your rash from amoxicillin in 2018 was truly an allergy or just a side effect. They don’t know if you’ve since outgrown it. And they rarely ask you to confirm it during check-ins.
That’s where the real problem lies. drug allergy alerts, automated warnings in EHRs triggered when a prescribed drug matches a patient’s recorded allergy. Also known as allergy decision support, they’re supposed to protect you are often ignored because they’re noisy, vague, or outdated. A 2023 study found that nearly half of all allergy alerts in primary care systems were triggered by non-specific terms like "drug reaction" instead of clear, actionable labels like "anaphylaxis to penicillin." Meanwhile, patients with documented severe allergies to drugs like carbamazepine or chloramphenicol—both linked to rare but deadly blood disorders—still get prescribed them when their allergy isn’t properly coded in the system. The fix isn’t just better tech. It’s better data. Clearer patient input. More training for staff to document allergies accurately. And systems that don’t just flash a warning, but ask: "Is this still true?"
What you’ll find in the posts below isn’t just theory. It’s real-world insight into how digital systems handle drug safety—from how nitrosamine contamination in generics gets flagged in EHRs, to why generic drug failure can be missed if allergy history isn’t tied to dosage records, to how FDA safety alerts for recalled medications should automatically update your EHR. You’ll see how pharmacies manage partial fills and back-orders without mixing up allergy-sensitive meds, and how patients can take control of their own allergy data to make sure it’s not lost in a system that’s supposed to protect them.
How to Update Your Allergy List Across All Healthcare Providers
Learn how to update your allergy list across all healthcare providers to prevent dangerous drug reactions. Get step-by-step tips for verifying, testing, and correcting your records-no matter which system your doctor uses.
About
Health and Medicine
Latest Posts


Coughs and Respiratory Infections: What to Watch Out For
By Orion Kingsworth Apr 23, 2025
Abiraterone: Transforming Prostate Cancer Care for African American Men
By Orion Kingsworth Oct 18, 2025

The Role of Calcipotriol in Treating Pustular Psoriasis
By Orion Kingsworth Nov 8, 2023