Healthcare Supply Chain: How Drug Availability, Quality, and Safety Connect
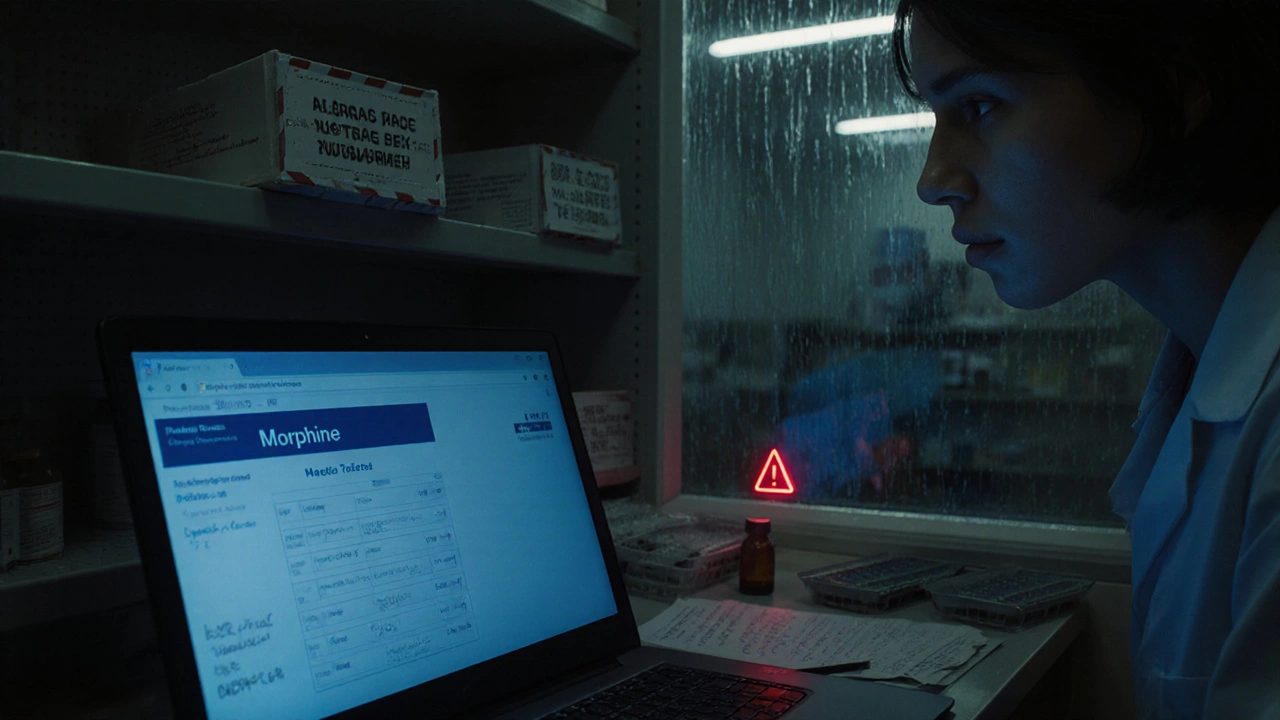
When you pick up a prescription, you’re not just getting a pill—you’re receiving the end result of a healthcare supply chain, the complex network that moves drugs from raw ingredients to patients. Also known as the pharmaceutical supply chain, it includes manufacturers, distributors, wholesalers, pharmacies, and regulators—all linked by timing, cost, and safety. Most people assume their medicine is safe because it’s on the shelf. But behind that assumption are real risks: contaminated ingredients, delayed shipments, and generic drugs made in factories with poor oversight.
The healthcare supply chain, the complex network that moves drugs from raw ingredients to patients. Also known as the pharmaceutical supply chain, it includes manufacturers, distributors, wholesalers, pharmacies, and regulators—all linked by timing, cost, and safety. The generic drugs, lower-cost versions of brand-name medications that must meet FDA bioequivalence standards. Also known as generic medications, they make up over 90% of prescriptions in the U.S. come mostly from overseas, especially India and China. China produces 80% of the world’s active drug ingredients, but FDA inspections have found widespread problems: fake data, dirty labs, and unapproved processes. That’s why over 500 drug recalls since 2018 involved nitrosamine contamination, cancer-causing impurities found in blood pressure and diabetes meds. Also known as NDMA, these chemicals slipped through because testing wasn’t required until after the damage was done. And when a batch fails, it doesn’t just sit on a warehouse shelf—it causes drug shortages, when a medication isn’t available in enough quantity to meet patient needs. Also known as medication shortages, they force doctors to switch treatments mid-course, sometimes with dangerous results.
It’s not just about where drugs come from—it’s about how they’re tracked. Pharmacies deal with partial fills and back-orders every day. One missed update in the system can mean a patient gets the wrong dose, or no dose at all. The pharmaceutical quality, the consistency and safety of a drug’s ingredients, manufacturing, and labeling. Also known as drug quality, it’s supposed to be guaranteed by the FDA—but inspections are rare, and enforcement is uneven. That’s why some patients report that their generic version doesn’t work like the last one. It’s not in their head. It’s because the active ingredient came from a different supplier, with different purity levels. Even authorized generics—identical to brand-name drugs but sold under a different label—can have different fillers or coatings that affect how the body absorbs them.
When you hear about a new FDA alert or a recall of a diabetes drug, it’s not random. It’s a symptom of a system under strain. The healthcare supply chain is fragile because it’s built on speed and low cost—not resilience. And when something breaks, patients pay the price. Below, you’ll find real stories and data on how these failures happen, who’s responsible, and what you can do to protect yourself—from nitrosamine-laced generics to stockouts that leave you without your life-saving meds. This isn’t theory. It’s what’s happening right now, in the medicine you trust.
Medication Shortages: How to Manage When Drugs Aren’t Available
Medication shortages are a growing crisis affecting hospitals, patients, and providers. Learn how to manage when critical drugs aren’t available, what’s causing the problem, and what you can do to protect patient care.
About
Health and Medicine
Latest Posts

Unlock the Secrets of Date Palm: The Ultimate Dietary Supplement for a Healthier You!
By Orion Kingsworth Jun 2, 2023

Benzodiazepines and Birth Defect Risks: What Pregnant Women Need to Know
By Orion Kingsworth Feb 7, 2026

GERD Management: Diet, Lifestyle, and Acid Reflux Medications
By Orion Kingsworth Dec 1, 2025