Why Starting Low and Going Slow Works Better for Your Body
Imagine starting a new medication and feeling sick within days-nausea, dizziness, fatigue-so bad you quit. That’s what happens when you jump straight to the full dose. But if you start with a tiny amount and slowly increase it over weeks, your body adapts. This isn’t guesswork. It’s science. And it’s why slow up-titration is now the standard for many of the most common chronic disease medications.
Take GLP-1 receptor agonists like semaglutide. At full dose, nearly two out of five people get severe nausea. But when doctors start at 0.25mg once a week and slowly bump it up every four weeks, that number drops to less than one in five. The same pattern holds for heart failure drugs like carvedilol and lisinopril. Patients who follow slow titration schedules are far more likely to stick with treatment-and far less likely to end up back in the hospital.
How Slow Up-Titration Actually Works
Your body doesn’t like sudden changes. When you take a powerful drug all at once, it hits receptors like a sledgehammer. Beta-blockers, for example, block adrenaline receptors. If you give the full dose right away, your heart rate plummets, blood pressure drops too fast, and you feel like you’re going to pass out. But if you start with 6.25mg twice a day and increase every two weeks, your body adjusts. Receptors downregulate gradually. Your blood vessels relax slowly. Your kidneys adapt.
This isn’t just about avoiding discomfort. It’s about survival. A landmark 1984 study found that only 12% of heart failure patients could tolerate full-dose metoprolol. But when titrated slowly, 83% stayed on it. Fast forward to today, and that same principle is used for diabetes drugs, high blood pressure meds, and even some psychiatric treatments. The goal isn’t to delay treatment-it’s to make it stick.
Real-World Titration Schedules You Need to Know
Not all slow titration is the same. The timeline depends on the drug and how it affects your body.
- GLP-1 agonists (semaglutide): Starts at 0.25mg weekly for 4 weeks, then 0.5mg for 4 weeks, then 1.0mg for 4 weeks. Only after 12 weeks do you consider 2.4mg. Total time to max dose: 16-20 weeks.
- Oral semaglutide: Begins at 3mg daily for 30 days, then 7mg for 30 days, then 14mg. That’s two full months before hitting the highest dose.
- Beta-blockers (carvedilol, metoprolol): Start at 3.125mg twice daily. Double every 2-4 weeks. Full dose usually reached in 8-12 weeks.
- ACE inhibitors (lisinopril): Begin at 2.5-5mg daily. Increase every 1-2 weeks until you hit 10-40mg daily, depending on kidney function and blood pressure.
- MRAs (spironolactone): Start at 12.5mg daily. Wait 4-8 weeks before increasing. Slower because of potassium risks.
These aren’t suggestions. They’re FDA-approved protocols backed by clinical trials. Skipping steps doesn’t speed up results-it increases the chance you’ll quit.
Why Some People Still Struggle-Even With Slow Titration
Slow titration helps, but it’s not magic. A 2021 study found that 22% of patients over 65 had trouble keeping track of changing doses. Some forgot when to increase. Others were scared to. One woman in Sydney told her pharmacist she didn’t want to risk the nausea again, so she stayed at 0.25mg for six months-even though her doctor had cleared her to move up.
Another issue? Side effects don’t always vanish. If nausea or dizziness lasts longer than two weeks at a given dose, don’t just push through. Call your doctor. That’s the rule of thumb. You might need a different drug, a lower dose, or extra support like anti-nausea meds.
And let’s be real: waiting months to feel the full benefit is frustrating. One Reddit user wrote: “I started semaglutide to lose weight. After 12 weeks, I’d lost 3 pounds. I almost quit.” But he didn’t. At 20 weeks, he’d lost 18. He’s now at 2.4mg and keeping it off.
What Happens When You Skip Titration
Some people think, “I’ll just start at the full dose and see what happens.” That’s risky. In the SUSTAIN FORTE trial, patients who rushed their semaglutide dose had a 45% chance of severe GI side effects. Those who followed the schedule? Just 18%.
And it’s not just nausea. Rapid titration of beta-blockers can cause low blood pressure, fainting, or even worsen heart failure in the short term. A 2019 analysis of the PARADIGM-HF trial showed that skipping titration steps increased severe adverse events by 52%.
There’s also the adherence problem. A 2021 JAMA study found that patients on full-dose regimens were 37% more likely to stop their meds within six months. Slow titration doesn’t just reduce side effects-it keeps you on the treatment that could save your life.
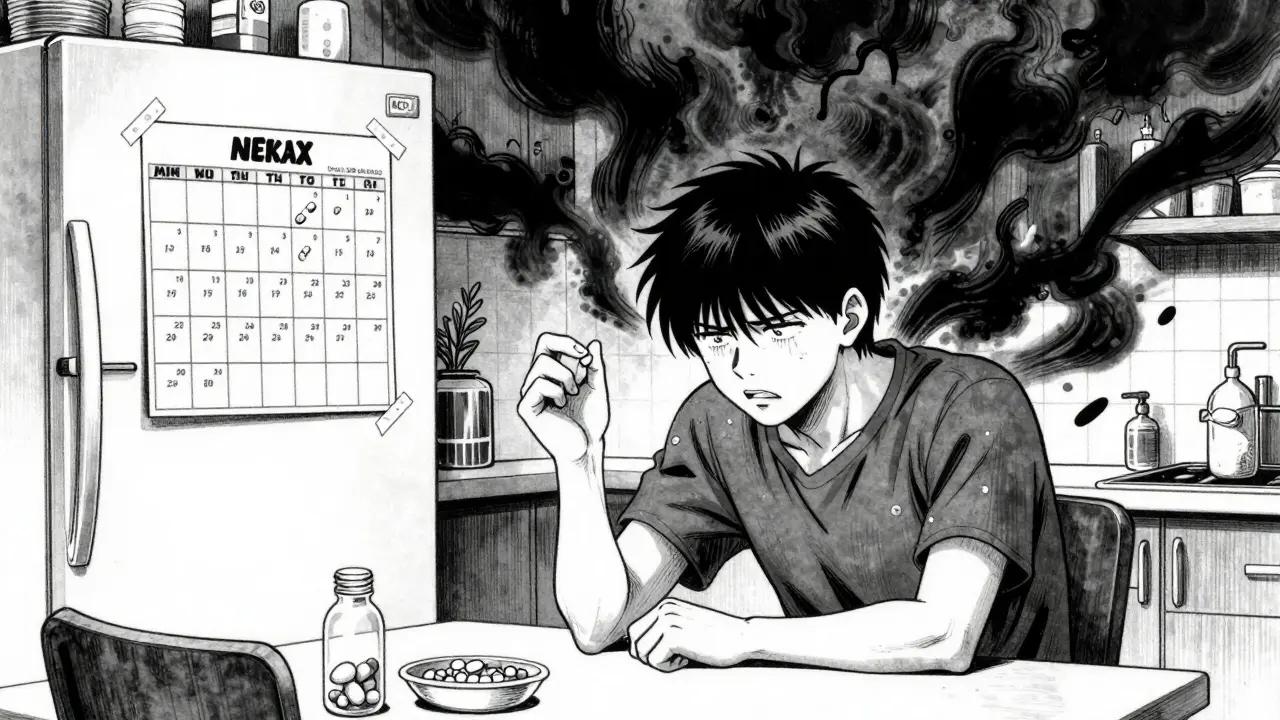
Tools and Tips to Make Titration Easier
You don’t have to manage this alone. Here’s what actually helps:
- Dose reminder apps: Medisafe and MyTherapy send alerts when it’s time to increase. Users report 18% better adherence.
- Written schedules: Ask your doctor for a printed titration calendar. Write the dates and doses in big letters. Tape it to your fridge.
- Weekly check-ins: Even a quick 5-minute phone call with your nurse can catch problems early. Many clinics now offer telehealth titration visits every two weeks.
- Keep a symptom journal: Note how you feel each day. Did the dizziness get better? Did your appetite return? That info helps your doctor decide when to increase.
One heart failure patient in Melbourne kept a simple notebook: “Week 4: No dizziness. Still a little tired. BP 120/78.” That’s all it took to confirm she was ready for the next step.
When Slow Titration Isn’t the Right Choice
Slow titration works best for long-term, chronic conditions. But it’s not for every situation.
For example, if you’re in the ER with a blood pressure of 220/120, you don’t want to wait 12 weeks to start lisinopril. You need labetalol or nitroprusside-fast-acting drugs that work immediately. Same goes for acute infections, severe pain, or sudden arrhythmias.
Even for chronic conditions, some drugs don’t need slow titration. SGLT2 inhibitors like dapagliflozin or empagliflozin can be started at full dose with minimal side effects. The 2023 DIAMOND trial showed no difference in safety between immediate and gradual starts for these drugs. So your doctor should tailor the plan-not just follow a blanket rule.

What Experts Are Saying
Dr. John McMurray, who helped write the European Heart Failure Guidelines, put it plainly: “Slow up-titration of quadruple therapy in heart failure improves outcomes. We’ve seen a 35% drop in deaths when patients follow the schedule.”
But not everyone agrees on how slow is too slow. Dr. Robert Lash from the American College of Endocrinology warns that for drugs like metformin-which are very safe-delaying the full dose can hurt. “If someone has an HbA1c of 10%, waiting 12 weeks to get to 1000mg twice daily is unnecessary. We’re letting blood sugar run high for no reason.”
The key takeaway? Slow titration isn’t one-size-fits-all. It’s a tool. Use it when the drug has a high risk of side effects. Skip it when the drug is forgiving.
What Comes Next: Personalized Titration
The future of titration is personal. Companies like Verily and Novo Nordisk are testing AI models that predict how you’ll respond to a drug based on your genes, weight, kidney function, and even gut bacteria. Early results show they can predict side effect risk 28% more accurately than standard methods.
For now, though, the best approach is still the old one: start low, go slow, listen to your body, and communicate with your care team. It’s not glamorous. But it works.
Millions of people have walked this path. They started scared. They felt sick. They almost quit. But they stuck with the schedule-and now they’re healthier than they’ve been in years.
How long does it usually take to reach the full dose with slow titration?
It depends on the medication. For GLP-1 agonists like semaglutide, it can take 16 to 20 weeks. For beta-blockers or ACE inhibitors, it’s often 8 to 12 weeks. Some drugs, like MRAs, may take up to 8 weeks just to reach the first increase. Always follow your doctor’s schedule-don’t rush it.
What if I feel fine at the low dose? Can I skip ahead?
Even if you feel fine, don’t skip steps. Side effects can be delayed. Your body is still adapting internally-your receptors, kidneys, and blood vessels are adjusting. Jumping ahead increases your risk of nausea, dizziness, low blood pressure, or even hospitalization. Stick to the plan.
Can I use over-the-counter meds to manage side effects during titration?
Some OTC options like ginger capsules or anti-nausea meds (dimenhydrinate) can help, but always check with your doctor first. Some OTC drugs can interact with your prescription-especially heart or kidney meds. Don’t self-treat without guidance.
What should I do if side effects last more than two weeks?
Contact your provider. The general rule is the “2-week rule”: if symptoms like nausea, fatigue, or lightheadedness don’t improve after two weeks at a given dose, it’s time to talk. You might need a dose adjustment, a different drug, or extra support-not just to push through.
Is slow titration only for older adults?
No. While older adults may need extra support to manage complex schedules, slow titration benefits people of all ages. Younger patients with diabetes or heart disease often benefit even more because they’re likely to be on the medication for decades. The goal is long-term safety, not just short-term comfort.
Final Thought: This Is About Staying on Treatment
The real win of slow up-titration isn’t that side effects disappear. It’s that you stay on the medicine that keeps you alive. Whether it’s your heart, your kidneys, or your blood sugar-this method gives your body time to adjust so you don’t have to quit. It’s not about speed. It’s about sustainability. And that’s what matters in the long run.


Jane Wei
December 17, 2025 at 18:14
I started semaglutide at 0.25mg and thought I was gonna puke every day. Turned out I just needed to eat a banana before the shot. No more nausea. Just sayin'.