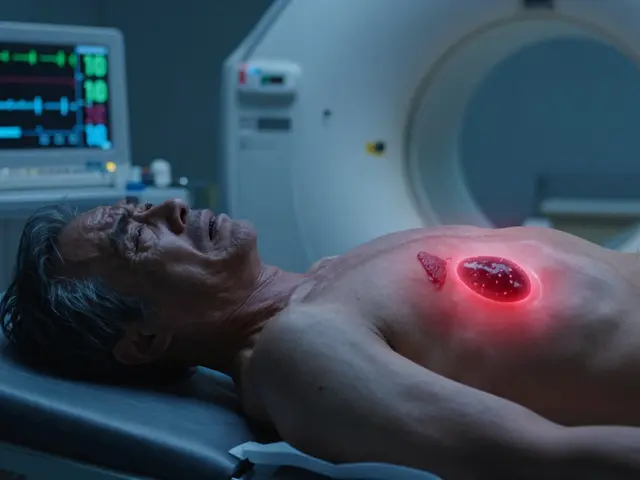
When your hip starts to ache with every step, it’s not just discomfort-it’s your body screaming that something’s off. For millions of people over 50, especially those carrying extra weight, that pain often comes from osteoarthritis of the hip. Unlike the more commonly discussed knee OA, hip osteoarthritis doesn’t always improve with simple fixes. But here’s the truth most doctors won’t tell you: losing weight isn’t just a suggestion-it’s one of the few proven ways to slow down joint damage and actually feel better.
Why Your Hip Hurts When You’re Overweight
Your hip joint is built to carry your whole body weight. Every time you walk, climb stairs, or even stand up from a chair, your hip bears three to six times your body weight. When you’re carrying extra pounds, that pressure piles up. Over time, the cartilage-the smooth cushion between your bones-wears down. Bone starts to rub on bone. Inflammation kicks in. Pain follows. It’s not just about mechanical stress, though. Fat tissue isn’t just padding-it’s active. It releases chemicals that trigger low-grade inflammation throughout your body, including your joints. That means even if you’re not putting more strain on your hip, your body is still attacking it from the inside. Studies show that people with a BMI over 30 are far more likely to develop hip osteoarthritis. And once it starts, the cycle gets worse: pain makes you move less, which leads to muscle loss, which makes movement even harder, which leads to more weight gain. It’s a loop, and breaking it starts with your weight.The Weight Loss Myth: Why Hip OA Is Different From Knee OA
You’ve probably heard that losing weight helps with knee arthritis. That’s true-and the evidence is rock solid. But hip osteoarthritis? The story gets messy. In 2023, NEJM Journal Watch published a blunt take: “Osteoarthritis of the Hips Is Unaffected by Weight Loss.” That headline made waves. And for a while, it felt like maybe dieting wasn’t worth the effort if your hip was the problem. But here’s what they didn’t say: that study looked at pain levels at six months. And then came the 2024 Nature study tracking 65-year-olds with hip OA and obesity. The results? People who lost more than 10% of their body weight saw a 31% improvement in their quality of life. Pain dropped. Mobility improved. Stiffness eased. The bigger the weight loss, the better the results. The key difference? Timing. Knee OA pain often improves within months. Hip OA takes longer. The 2023 clinical trial that showed no pain difference at six months? At 12 months, the group that lost weight had significantly better function and less pain than those who only exercised. Your hip doesn’t heal fast-but it does heal if you give it time and enough weight loss.How Much Weight Do You Actually Need to Lose?
Forget the 5% rule. That number came from knee OA studies. For your hip, the data points to a higher target. - Less than 5% weight loss? Minimal change in symptoms.- 5-7%? Some improvement in stiffness and daily movement.
- 7-10%? Clear, measurable improvement in pain and function.
- Over 10%? Major gains-up to 31% better quality of life, according to the Nature study. One Australian program, the Osteoarthritis Healthy Weight For Life (OAHWFL), targets 7-10% weight loss over 18 weeks. Participants didn’t just lose weight-they regained the ability to walk without pain, get out of bed without help, and even play with their grandkids again. And here’s the kicker: losing 20% didn’t give you much more benefit than losing 10%. That means you don’t need to become skinny. You just need to lose enough to take the pressure off.
What Works: Diet, Exercise, and the Right Combo
You can’t just diet. You can’t just exercise. You need both. A 2023 trial compared two groups: one did a very-low-calorie diet plus exercise, the other did exercise alone. The diet group lost 8.5% more weight. At six months, pain levels were almost the same. But at 12 months? The diet-plus-exercise group had better hip function, less pain, and improved walking speed. Why? Because exercise rebuilt the muscles around the hip. Diet reduced the load. Together, they protected the joint. The best plan? A low-carb or Mediterranean-style diet paired with strength training. Focus on:- Reducing sugar and refined carbs-these spike inflammation.
- Eating more vegetables, lean protein, and healthy fats-these reduce swelling.
- Doing seated leg lifts, glute bridges, and resistance band walks-these strengthen the hip without pounding the joint.
Real Results: What Happens When People Actually Lose Weight
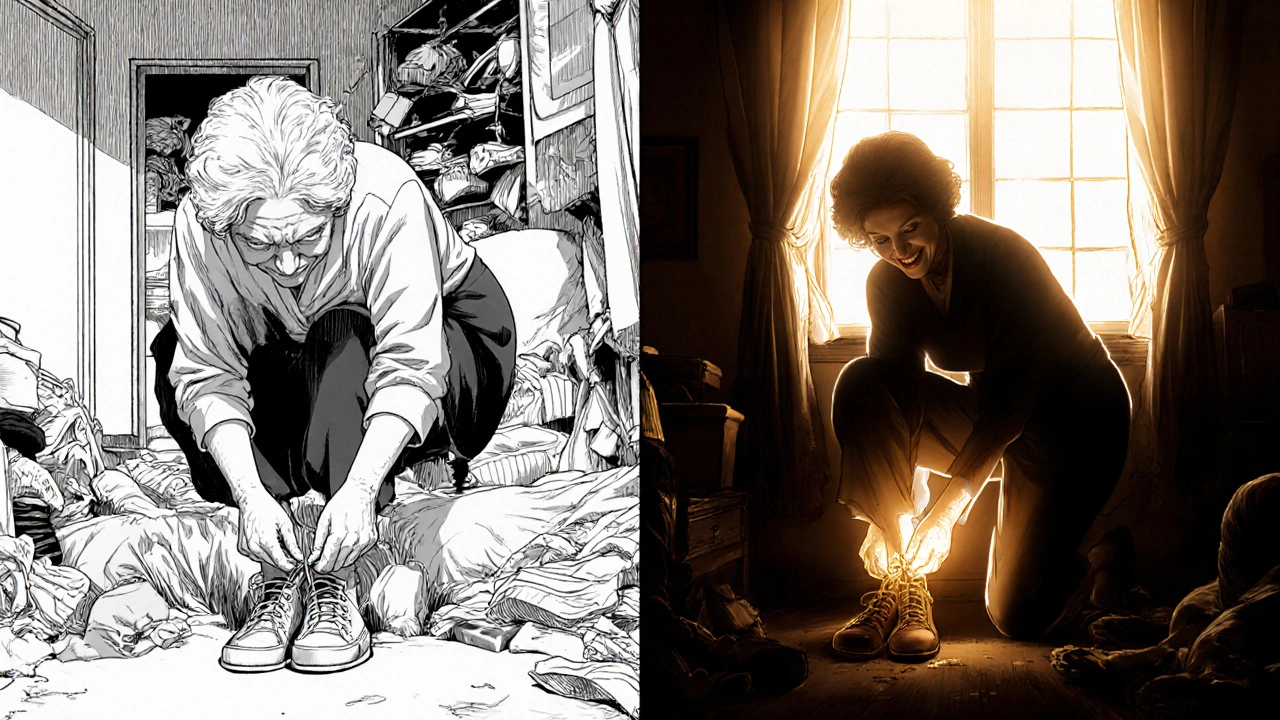
In a 2012 study, 35 people with hip OA and a BMI over 25 followed an eight-month program of diet and exercise. They lost an average of 10% of their body weight. What happened next? - 32.6% improvement in physical function (measured by WOMAC scores).- Pain dropped by nearly half.
- Walking speed increased by 20%.
- Many stopped needing painkillers. One participant, a 68-year-old woman from Sydney, told researchers she hadn’t been able to tie her shoes in three years. After the program, she did it without help. “I didn’t think I’d ever get that back,” she said. These aren’t outliers. They’re what happens when you treat hip OA like a lifestyle disease-not just a joint problem.
What About Weight Loss Drugs?
If you’ve tried everything and still can’t lose the weight, medications like semaglutide or tirzepatide are now approved for obesity in people with BMI over 30. But here’s the catch: they’re not first-line. The American College of Rheumatology says you should try diet and exercise for at least six months before considering them. Why? Because drugs help you lose weight. But only lifestyle changes help you keep it off-and rebuild the muscles that protect your hip. Medications are a tool, not a fix. Also, they’re expensive. And not everyone qualifies. For most people, the real solution is still food, movement, and consistency.




steffi walsh
November 17, 2025 at 22:27
Just started walking 10 mins after dinner like the post said and already feel less stiff in the morning. Not magic, but it’s something. Small wins count.