Naloxone with Opioids: How It Works and Why It Saves Lives
When someone overdoses on naloxone with opioids, a life-saving medication that blocks opioid receptors in the brain to reverse respiratory depression. Also known as Narcan, it’s not a treatment for addiction—it’s an emergency tool that brings someone back from the edge of death. Every year, tens of thousands of people in the U.S. die from opioid overdoses. Many of those deaths could be prevented if naloxone was available and used quickly.
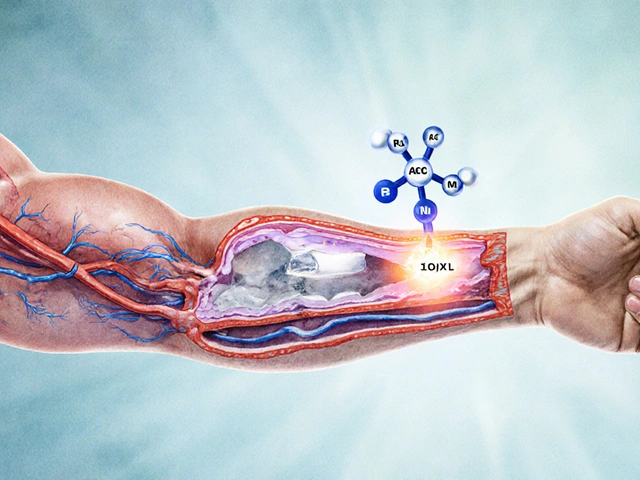
Opioid overdose, a condition where breathing slows or stops due to too much opioid in the system. Also known as respiratory depression, it’s the leading cause of death in drug overdoses. Opioids like heroin, fentanyl, oxycodone, and even prescription painkillers can shut down breathing. The body can’t handle the overload. That’s where naloxone steps in—it binds to the same receptors as the opioid but doesn’t cause any high or sedation. Instead, it kicks the opioid off and lets the person breathe again. It works in under two minutes when given as a nasal spray or injection.
But naloxone isn’t magic. It only lasts 30 to 90 minutes. Many opioids, especially fentanyl, last much longer. That means someone can overdose again after naloxone wears off. That’s why calling 911 is just as important as giving the dose. Emergency help is needed even if the person wakes up. And if you’re taking opioids regularly—whether for pain or otherwise—keeping naloxone on hand isn’t just smart, it’s a safety net. Family members, friends, and even coworkers should know where it is and how to use it.
Naloxone reversal, the process of restoring normal breathing after an opioid overdose using naloxone. Also known as opioid reversal, it’s one of the few medical interventions that can be done by someone with no training. Training programs are available in pharmacies, community centers, and online. Most states allow naloxone to be bought without a prescription. It’s cheap, safe, and has almost no side effects—unless the person is dependent on opioids. Then they might get sick right away: nausea, sweating, agitation. That’s not an allergic reaction. That’s withdrawal. And it’s better than being dead.
There’s a myth that giving naloxone encourages drug use. It doesn’t. Studies show people who receive naloxone are more likely to seek treatment afterward. It doesn’t fix addiction—but it gives someone another chance to try. And in a crisis, that chance is everything.
The posts below cover the real-world details you need: how naloxone interacts with other drugs, why some overdoses need multiple doses, what to do after giving it, and how it fits into broader opioid safety. You’ll find stories from people who’ve used it, data on its effectiveness, and warnings about hidden risks—like mixing it with other sedatives. This isn’t theoretical. These are the tools and truths that keep people alive.
Naloxone Co-Prescribing: How It Prevents Opioid Overdoses in Patients on Pain Meds
Naloxone co-prescribing saves lives by giving opioid patients a safety net against overdose. Learn who needs it, how it works, and how to get it-even without a prescription.
About
Health and Medicine
Latest Posts

Movfor (Molnupiravir) vs Alternatives: A Practical Comparison
By Orion Kingsworth Oct 14, 2025

Understanding Priligy Tablets for Premature Ejaculation Treatment: A Comprehensive Drug Guide
By Orion Kingsworth Mar 22, 2024
Experience the Magic of Kombucha Tea: Nature's Most Potent Dietary Supplement
By Orion Kingsworth Jun 12, 2023

