Narrow Therapeutic Index: What It Means and Why It Matters for Your Medications
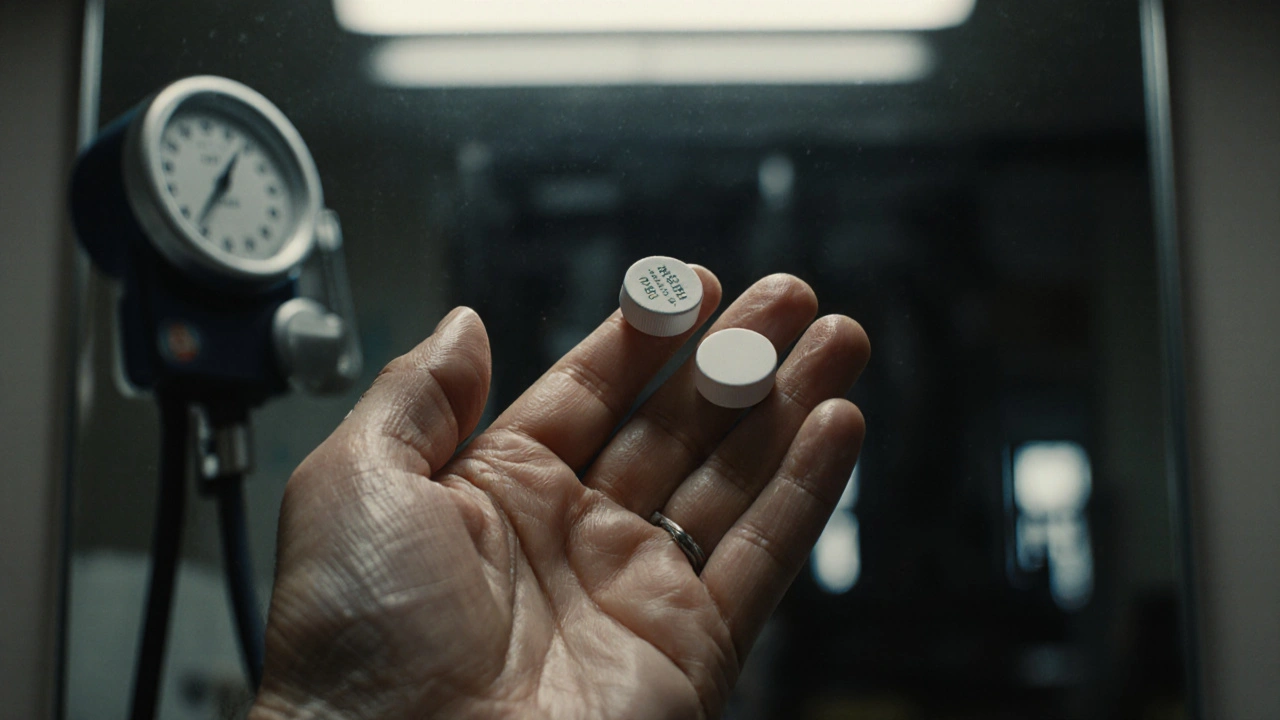
When a drug has a narrow therapeutic index, the range between an effective dose and a toxic dose is very small. Also known as a narrow therapeutic window, this means even a tiny change in dosage can cause serious harm—or make the drug useless. Think of it like walking a tightrope: too little, and the treatment doesn’t work; too much, and you risk poisoning yourself. This isn’t theoretical—it’s a daily concern for people taking drugs like warfarin, lithium, phenytoin, or digoxin. These aren’t rare meds. They’re used for heart conditions, seizures, mental health, and blood clots. And if you’re on one, you need to know how fragile the balance is.
That’s why generic drugs, medications that copy brand-name versions after patents expire can be tricky here. While most generics are safe and effective, those with a narrow therapeutic index demand near-perfect consistency. A 5% difference in absorption might be fine for an allergy pill, but for lithium, it could send your blood levels from safe to dangerous. That’s why some doctors insist you stick with the same brand or manufacturer—even if the generic is cheaper. The FDA says generics must be bioequivalent, but bioequivalence doesn’t always mean identical in real life. That’s why you see recalls for nitrosamine contamination or manufacturing flaws in generics—it’s not just about purity, it’s about how your body reacts to every milligram.
Bioequivalence, how closely a generic matches the original in how it’s absorbed and used by the body becomes critical here. Studies show that for drugs like warfarin, switching between generics can lead to spikes in INR levels—raising your risk of bleeding. That’s not a fluke. It’s a pattern. And it’s why pharmacists are trained to flag these meds for extra review. You might think all pills with the same name are interchangeable, but with a narrow therapeutic index, they’re not. Your body remembers the exact formulation. Even small changes in fillers, coatings, or release rates can throw off your balance.
This isn’t just about pills. It’s about how your care team manages your meds. Are they checking blood levels regularly? Are they aware of your full list of drugs? A simple interaction—like starting a new antibiotic or switching from one antiseizure drug to another—can tip the scale. That’s why medication shortages, partial fills, or back-orders aren’t just inconveniences. For someone on a narrow therapeutic index drug, they’re risks. A delay in refill or a switch to a different generic without monitoring could mean a trip to the ER.
What you’ll find below are real-world stories and guides from people who’ve walked this line. You’ll learn how to spot when a generic switch might be unsafe, how to talk to your pharmacist about your meds, what to do if you’re told your drug is on shortage, and why some doctors refuse to let you switch brands. These aren’t abstract theories. They’re lessons from patients who’ve been there—and from pharmacists who’ve had to fix the mistakes.
Therapeutic Failures: When a Generic Drug Doesn't Work as Expected
Generic drugs are supposed to be safe, affordable copies of brand-name meds - but when they fail, the results can be deadly. Learn why some generics don’t work as expected and what you can do to protect yourself.
About
Medications
Latest Posts


The Relationship Between Bisoprolol Fumarate and Anxiety
By Orion Kingsworth Apr 27, 2023

Buy Ampicillin Online Safely: A 2025 Australian Guide
By Orion Kingsworth Aug 11, 2025

Opioid-Induced Itching: How Histamine and Nerve Pathways Trigger It and What Actually Works
By Orion Kingsworth Oct 30, 2025