POTS Syndrome – What You Need to Know
Postural Orthostatic Tachycardia Syndrome (POTS) is a condition where standing makes your heart race and can leave you feeling dizzy or exhausted. It isn’t rare, but many people never hear the name until symptoms hit. Understanding the basics helps you spot it early and get the right help.
The core problem is an abnormal response of the autonomic nervous system to gravity. When you go from lying down to standing, blood pools in your legs, and instead of adjusting smoothly, your heart speeds up dramatically—often over 30 beats per minute within ten minutes. This surge can trigger headaches, brain fog, or even fainting.
Common Symptoms of POTS
The symptoms vary, but most people notice a few key signs: rapid heartbeat on standing, light‑headedness, and extreme fatigue that doesn’t improve with rest. Some also report trouble concentrating, nausea, or cold feet. The symptoms often worsen after meals, in hot weather, or during long periods of sitting followed by standing.
Because the list is long, doctors sometimes miss POTS or label it as anxiety. If you’ve tried drinking more water or caffeine and still feel off, it’s worth asking a clinician about a tilt‑table test—a standard way to confirm the diagnosis.
How Doctors Diagnose POTS
A doctor will first review your medical history and run basic blood work to rule out anemia, thyroid issues, or dehydration. The definitive step is the standing test: you lie down for ten minutes, then stand while heart rate and blood pressure are measured for at least ten more minutes.If the heart rate climbs by 30 beats per minute (or hits over 120 bpm) without a significant drop in blood pressure, it meets the criteria for POTS. Some specialists also check for related conditions like Ehlers‑Danlos syndrome or mast cell activation, which can influence treatment choices.
Managing POTS in Everyday Life
Lifestyle tweaks make a big difference. Start each day with 2–3 liters of water and add a pinch of salt (if your doctor approves) to boost blood volume. Compression socks or leggings help keep blood from pooling in the lower body.
Exercise might sound scary, but gradual, low‑impact workouts—like recumbent cycling or swimming—strengthen the leg muscles that push blood back up. Aim for short sessions a few times a week and increase duration slowly.
Meal planning also matters. Smaller, frequent meals with balanced carbs and protein prevent the post‑meal dip in blood pressure. Avoid large amounts of alcohol and limit caffeine to early morning if it makes you jittery later.
If symptoms stay severe, medication can assist. Options include beta‑blockers to tame heart rate spikes, fludrocortisone to raise blood volume, or midodrine to tighten blood vessels. Always discuss benefits and side effects with a healthcare provider.
Lastly, track your day in a simple journal: note when you feel worst, what you ate, how much you moved, and any meds taken. Patterns emerge quickly, and you can share the data with your doctor for smarter adjustments.
POTS is manageable once you understand its triggers and have a plan. By staying hydrated, moving smartly, and working with a clinician, you can reduce flare‑ups and reclaim everyday energy.
Amlodipine and POTS Syndrome: Can This Medication Help with Symptoms?
In my recent blog post, I explored the potential benefits of Amlodipine for individuals with POTS Syndrome. I discovered that this medication, typically used to treat high blood pressure, has shown some promise in alleviating symptoms for some POTS patients. However, it's important to note that the results vary between individuals and it may not work for everyone. I strongly recommend speaking with your doctor if you're considering trying Amlodipine for your POTS symptoms. As always, it's crucial to weigh the potential risks and benefits before starting any new treatment plan.
About
Health and Medicine
Latest Posts


Dapagliflozin: FAQ, Guide, and Expert Answers for Diabetes and Heart Health
By Orion Kingsworth May 9, 2025
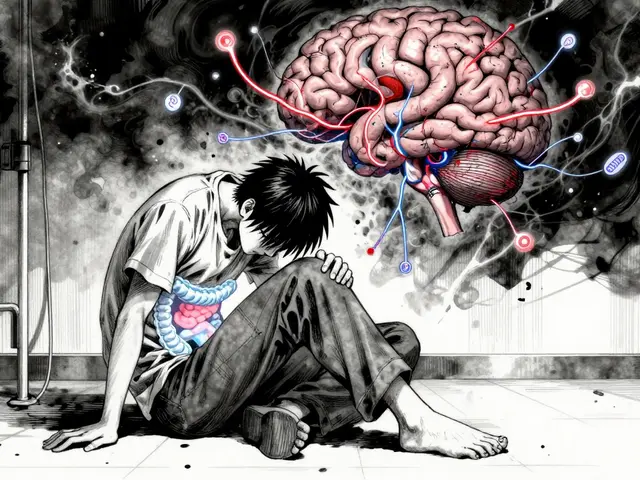
Irritable Bowel Syndrome: How the Gut-Brain Axis Causes Symptoms and How to Find Relief
By Orion Kingsworth Dec 22, 2025

The Role of Calcipotriol in Treating Pustular Psoriasis
By Orion Kingsworth Nov 8, 2023

