When your child tugs at their ear, cries more than usual, or won’t sleep through the night, it’s easy to jump to one conclusion: ear infection. And in many cases, you’re right. About 83% of kids have at least one ear infection by age 3. But here’s what most parents don’t know - the best treatment isn’t always antibiotics. Sometimes, waiting is the smartest move.
What Exactly Is an Ear Infection?
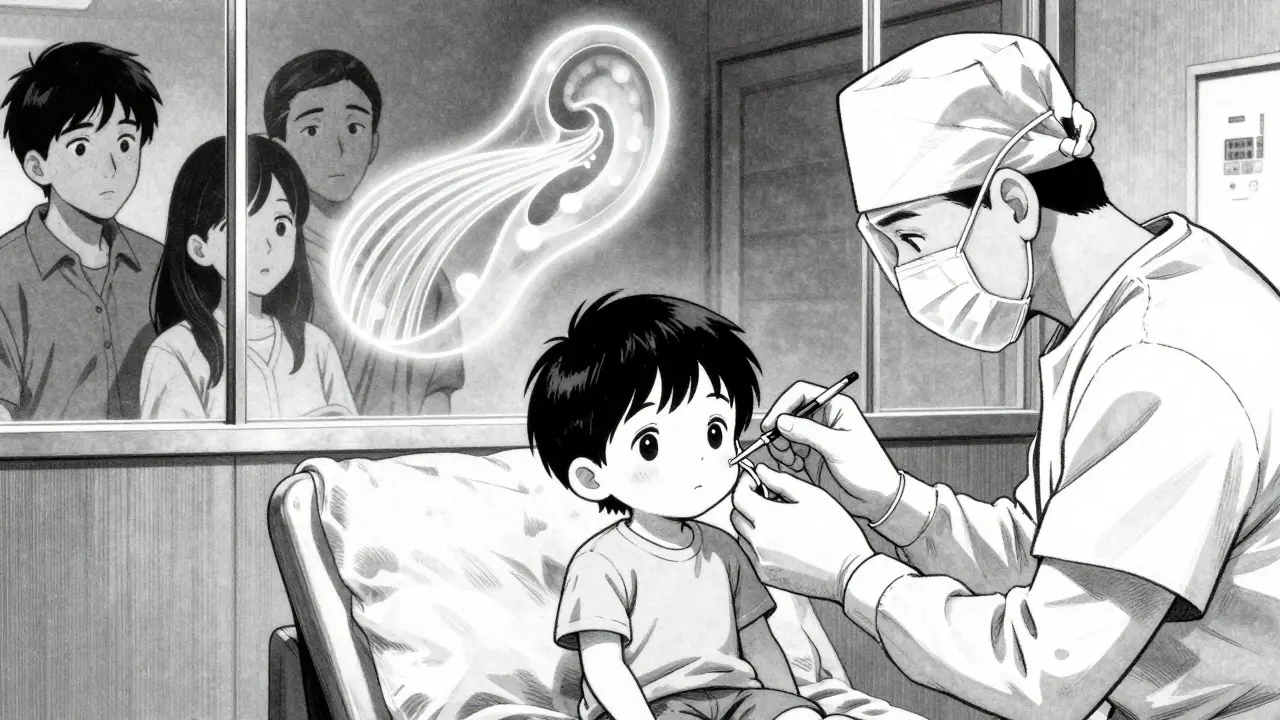
An acute ear infection, or acute otitis media (AOM), isn’t just fluid behind the eardrum. It’s an active infection with clear signs: a bulging, red eardrum, pain, and often fever. Doctors diagnose it using a special tool called an otoscope to check for inflammation and fluid buildup. The key is that all three things must be present - sudden onset, fluid, and signs of infection. If your child has fluid but no redness or pain, it’s not an active infection. That’s called otitis media with effusion, and it doesn’t need antibiotics.
Most ear infections happen between 6 and 24 months. Why? Their Eustachian tubes - the little channels connecting the middle ear to the back of the throat - are shorter and more horizontal than adults’. That makes it easier for germs from colds to travel up and get trapped. Kids in daycare, those exposed to smoke, or those who bottle-feed while lying down are at higher risk.
Antibiotics: Not Always the Answer
For decades, antibiotics were the default treatment. But overprescribing led to a bigger problem: antibiotic resistance. Today, the CDC estimates that 2.8 million antibiotic-resistant infections happen every year in the U.S. - and ear infections are a big part of that.
Current guidelines from the American Academy of Pediatrics say antibiotics aren’t needed for every case. In fact, 60 to 80% of ear infections clear up on their own within a few days. So when do you really need them?
- Yes, antibiotics right away: Babies under 6 months, kids with severe pain or fever over 102.2°F (39°C), or anyone with drainage from the ear (otorrhea).
- Wait and watch: Kids 6 to 23 months with mild symptoms and only one infected ear. Kids 2 years and older with mild symptoms, even if both ears are affected.
High-dose amoxicillin is still the first-line treatment - 80 to 90 mg per kilogram of body weight daily. For kids allergic to penicillin, alternatives like cefdinir or clindamycin are used. The course length depends on age: 10 days for toddlers under 2, 7 days for ages 2 to 5, and just 5 days for kids 6 and older with mild cases.
But here’s the catch: even when antibiotics are prescribed, pain control is just as important. Studies show that 69% of kids with ear infections have significant pain - yet only 37% get proper pain relief. Give acetaminophen or ibuprofen (if over 6 months old) on a regular schedule, not just when the pain spikes. Don’t wait for the fever to spike before giving medicine. Pain management is the real first step in treatment.
Watchful Waiting: A Proven Strategy
Watchful waiting isn’t ignoring the problem - it’s a structured plan. You give your child pain relief and monitor closely. If symptoms don’t improve in 48 hours, or if they get worse, you start the antibiotics.
Parents are often nervous about this approach. But data backs it up. In studies, only about one-third of kids who started with watchful waiting ended up needing antibiotics. Most improved on their own within 24 to 48 hours. And there’s no increase in complications like ruptured eardrums or hearing loss.
Doctors often give a safety-net prescription - a paper or digital script you only fill if symptoms don’t improve. This gives parents peace of mind without rushing to antibiotics. In clinics that use this system, 76% of families follow through with the plan, and antibiotic use drops by 35% compared to old practices.
What to watch for:
- Ear pain lasting more than 48 hours
- Fever over 102.2°F (39°C)
- Drainage from the ear
- Refusal to eat or drink
- Extreme fussiness or lethargy
If any of these happen, call your doctor. Don’t wait. But if your child is still feeding, sleeping, and acting mostly like themselves, give it time.

When Tubes Become Necessary
Some kids get ear infections over and over. That’s called recurrent AOM. If your child has three infections in six months, or four in a year - with at least one in the last six months - it’s time to talk about tubes.
Tympanostomy tubes are tiny cylinders placed through the eardrum during a quick outpatient surgery. They let air into the middle ear, preventing fluid buildup and reducing infection risk. Tubes usually fall out on their own after 6 to 18 months.
But tubes aren’t for every kid who gets frequent ear infections. The AAP says you need documented hearing loss (at least 40 dB) or persistent fluid for three months before considering them. Many kids get tubes too early - because parents and doctors are frustrated, not because it’s medically needed.
Studies show tubes cut infection rates by about half in the first six months after placement. But after that, the benefit fades. And there are risks: scarring of the eardrum, long-term perforation, or the need for repeat surgery.
Also, tubes don’t fix hearing loss caused by fluid if it’s not severe. If your child’s hearing is normal between infections, tubes won’t help them learn to talk better. Speech delays are more often tied to long-term fluid buildup - not just frequent infections.
Before agreeing to tubes, ask: Has hearing been tested? Is there fluid that won’t go away? Has my child had at least one infection in the last six months? If the answer is no to any of these, wait.
What Doesn’t Work
There’s a lot of misinformation out there. Many parents try decongestants, antihistamines, or nasal sprays. But research shows they don’t help. In fact, they can cause drowsiness, irritability, or even dangerous side effects in young kids.
Home remedies like warm oil drops, garlic, or herbal sprays? No evidence they work. And putting anything in the ear canal can damage the eardrum if it’s already inflamed.
And while vaccines won’t prevent every ear infection, the pneumococcal conjugate vaccine (PCV13) has helped. Since it became routine in 2010, ear infections dropped by 12%, and recurrent cases fell by 20%. That’s a real win.
What’s Changing in 2025
Guidelines are still being updated. The latest draft from the AAP, expected to be finalized in 2025, will make watchful waiting even more common. For the first time, it may recommend delaying antibiotics for some two-year-olds with bilateral ear infections - if symptoms are mild.
Doctors are also being pushed to use better tools. Electronic health records now include prompts that remind clinicians to check for pain severity and to offer safety-net prescriptions. In clinics that use these tools, antibiotic prescribing dropped by nearly 30%.
But the biggest barrier isn’t medical - it’s parental pressure. One in two parents asks for antibiotics, even when the doctor says it’s not needed. And many doctors give in because they’re short on time or don’t want to upset a family. That’s why education matters. If you understand the science, you can advocate for your child without pushing for drugs.
What to Do Next
If your child has an ear infection:
- Give pain relief - acetaminophen or ibuprofen - on a regular schedule.
- Watch for improvement over 48 hours.
- Call the doctor if symptoms worsen or don’t improve.
- Ask: Is this a severe case? Is my child under 6 months? Is there drainage?
- If it’s mild and your child is over 2, ask about watchful waiting.
- If infections keep coming, ask for a hearing test before agreeing to tubes.
Ear infections are common. But they don’t have to be treated the same way every time. The goal isn’t to eliminate every infection - it’s to protect your child’s hearing, avoid unnecessary drugs, and let their body heal when it can.
Do all ear infections need antibiotics?
No. About 60% to 80% of ear infections in children clear up on their own within a few days. Antibiotics are only needed for severe cases, babies under 6 months, or if symptoms don’t improve after 48 hours of watchful waiting and pain relief.
Can ear infections cause hearing loss?
Temporary hearing loss can happen if fluid builds up behind the eardrum and stays for weeks or months. This is called otitis media with effusion. If it lasts longer than three months and affects speech or learning, it needs medical attention. Permanent hearing loss from ear infections is rare.
Are ear tubes safe for young kids?
Yes, tubes are generally safe and are one of the most common childhood surgeries. They reduce infection frequency in the first six months and help with fluid drainage. But they’re not a cure-all. Risks include scarring of the eardrum or the need for repeat surgery. They should only be considered after documented hearing loss or persistent fluid.
How long do ear tubes last?
Most ear tubes fall out on their own between 6 and 18 months after placement. The eardrum usually heals naturally after they come out. In rare cases, tubes may stay longer or require removal, but this happens in less than 5% of cases.
Can I prevent ear infections in my child?
You can reduce the risk. Breastfeeding for at least six months, avoiding secondhand smoke, keeping your child up to date on vaccines (especially PCV13), and limiting pacifier use after 6 months all help. Kids in daycare are more likely to get infections, but that’s normal as their immune system learns.



mukesh matav
December 22, 2025 at 07:10
My nephew had three ear infections in six months. We went the watchful waiting route after the second one. Turned out he was fine by day three each time. Pain meds and patience beat antibiotics every time.