Diabetes and Steroids: How Steroids Affect Blood Sugar and What to Do
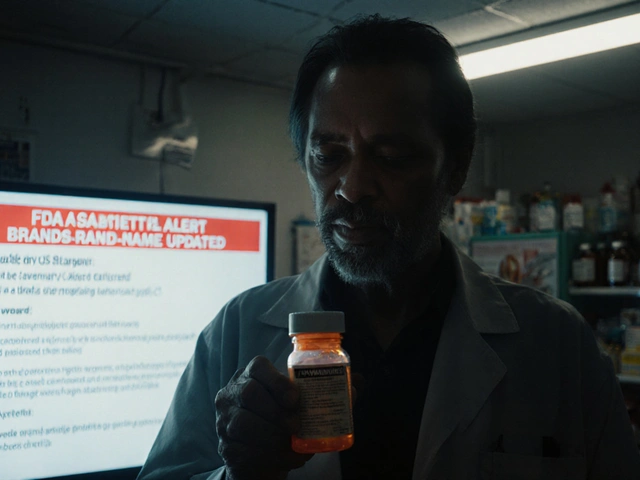
When you have diabetes, a condition where the body struggles to regulate blood sugar, taking steroids, powerful anti-inflammatory drugs like prednisone or dexamethasone can throw your whole system off. These drugs don’t just reduce swelling or calm an autoimmune flare—they also tell your liver to pump out more glucose, while making your muscles and fat cells less responsive to insulin. The result? Blood sugar levels climb, sometimes dangerously high, even in people who never had diabetes before. This isn’t a side effect you can ignore. It’s a direct, measurable shift in how your body handles sugar—and it happens fast.
If you’re on steroids for asthma, rheumatoid arthritis, or even a bad allergic reaction, your doctor might not warn you about this. But if you have type 2 diabetes, prediabetes, or a family history of it, you’re at higher risk. Some people see their fasting blood sugar jump from 100 to 200 mg/dL within days of starting a steroid course. Insulin needs can double or triple. You might feel hungrier, thirstier, or need to pee more often. These aren’t just annoyances—they’re warning signs. And if you’re not tracking your numbers, you could end up in the hospital with diabetic ketoacidosis, even if you’ve been managing your diabetes fine for years.
It’s not just about taking more insulin. You need to adjust your diet, timing of meals, and activity levels too. Steroids often cause sugar spikes in the afternoon and evening, so checking your blood sugar at those times matters more than ever. Some people need to switch from oral meds to insulin temporarily, while others just need tighter carb control. There’s no one-size-fits-all fix, but you can’t wing it. The blood sugar control, the ability to keep glucose levels within a safe range becomes a daily battle when steroids are in the picture. And if you’re on long-term steroids, like for lupus or COPD, this isn’t a short-term problem—it’s a permanent part of your care plan.
You’ll find real stories and practical advice in the posts below. Some people had to restart insulin after years off. Others learned how to time their meals around steroid doses. One person discovered their blood sugar spiked every time they took prednisone at night. These aren’t theoretical concerns—they’re lived experiences. Whether you’re a patient, a caregiver, or a healthcare provider, you need to know how steroids interact with diabetes. This isn’t about avoiding steroids. It’s about using them safely when you need them. The tools, tips, and warnings in these posts are built from real cases, not guesswork. You’ll see how others managed it—and what worked when things got messy.
Steroid Hyperglycemia in Diabetes: How to Adjust Insulin and Medications
Steroid hyperglycemia can spike blood sugar in diabetics and even trigger new-onset diabetes. Learn how to adjust insulin doses, monitor glucose, and avoid dangerous lows during steroid tapering with expert-backed strategies.
About
Medications
Latest Posts

Hypoparathyroidism: How to Manage Low Calcium and Vitamin D Effectively
By Orion Kingsworth Dec 5, 2025

The Use of Minocycline in Treating Prostatitis
By Orion Kingsworth May 21, 2023

How to Create a Medication Plan Before Conception for Safety
By Orion Kingsworth Jan 6, 2026

