Geriatric Assessment: What It Is and Why You Need It
If you or a loved one is 65 or older, you’ve probably heard the term “geriatric assessment” tossed around in doctors’ offices. It’s not just a fancy label – it’s a step‑by‑step check‑up that looks at the whole person, not just a single disease. The goal is simple: spot problems early, keep independence, and avoid hospital trips.
Think of it as a health report card for seniors. Instead of grading you on math, it grades you on mobility, memory, medication safety, nutrition, and social support. By gathering all that info in one place, doctors can create a plan that fits your real life, not just the textbook version of aging.
Why a Geriatric Assessment Matters
Older adults often juggle several health issues at once – high blood pressure, arthritis, mild memory lapses, and maybe a few pills they can’t remember taking. A standard visit might miss how these pieces affect each other. A geriatric assessment pieces the puzzle together.
Research shows that seniors who get a full assessment are less likely to fall, have fewer medication errors, and stay in their homes longer. It also gives families a clear picture of what to expect, so they can plan support early rather than scrambling when a crisis hits.
Key Components of a Comprehensive Geriatric Assessment
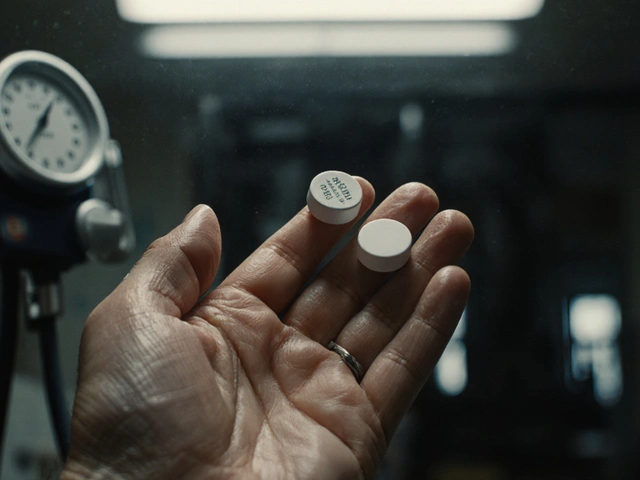
1. Medical Review – The doctor looks at all current conditions, past surgeries, and the medication list. This is the time to ask why you’re on each drug and whether any can be stopped.
2. Functional Check – Simple tasks like getting out of a chair, climbing stairs, or buttoning a shirt are tested. These results tell whether you might need a grab bar, a walking aid, or home modifications.
3. Cognitive Screening – A quick memory game or questionnaire spots early signs of dementia. Catching it early means you can start strategies to keep your mind sharp.
4. Mood and Social Support – Feeling down or isolated can worsen physical health. The assessment asks about mood, friendships, and whether you have someone to call when you need help.
5. Nutrition Review – Malnutrition is a hidden danger for seniors. The team checks weight trends, appetite, and whether you’re getting enough protein and vitamins.
After these steps, the team (often a doctor, nurse, therapist, and social worker) puts together an action plan. It might include adjusting meds, setting up physical therapy, arranging meal delivery, or connecting you with a community group.
Getting a geriatric assessment doesn’t have to be a big hassle. Many clinics schedule it as a half‑day visit, and some home‑health agencies can do it at your doorstep. If you see any of the warning signs – frequent falls, confusion, new medication side effects, or feeling lonely – reach out to your primary care doctor and ask about a geriatric assessment.
Remember, the aim is to keep you living safely and happily, not just to add more appointments. A thorough check‑up gives you and your family the confidence to make everyday decisions without fear. So, the next time you hear “geriatric assessment,” think of it as a personalized health roadmap, not just another test.
Lymphoma in the Aging Population: Key Challenges & Practical Considerations
Explore how lymphoma affects older adults, the unique medical hurdles they face, and actionable strategies for clinicians and caregivers.
About
Health and Medicine
Latest Posts

Seasonal Affective Disorder: How Light Therapy Helps with Winter Depression
By Orion Kingsworth Feb 2, 2026

Authorized Generics: Same Drug, Different Label - What You Need to Know
By Orion Kingsworth Jan 7, 2026
The Environmental Impact of Eflornithine Production
By Orion Kingsworth Oct 30, 2025

