Obesity and Arthritis: How Excess Weight Worsens Joint Pain and What You Can Do
When you carry extra weight, your obesity and arthritis, a condition where excess body fat increases mechanical stress and systemic inflammation on joints. Also known as weight-related joint disease, it’s not just about worn-out cartilage—it’s about your body’s chemistry turning against you. Every pound you carry adds 3 to 4 pounds of pressure on your knees. That means someone who’s 50 pounds overweight is putting 150 to 200 extra pounds of force on their joints with every step. Over time, this crushes the cushioning between bones, leading to osteoarthritis—the most common form of joint degeneration.
But it’s not just physical pressure. Fat tissue isn’t just storage—it’s active. inflammation from excess fat, a chronic, low-grade immune response triggered by adipose tissue releasing harmful proteins. Also known as meta-inflammation, it floods your bloodstream with cytokines that attack joint linings, making pain worse even in hips, hands, and spine. Studies show people with obesity have higher levels of interleukin-6 and TNF-alpha—chemicals directly linked to cartilage breakdown. This is why two people with the same level of joint wear can have wildly different pain levels: one has extra fat fueling the fire.
That’s why weight loss for arthritis, a proven strategy to reduce joint stress and lower inflammatory markers. Also known as metabolic joint intervention, it’s not just about looking better—it’s about getting back on your feet without relying on stronger painkillers. Losing just 10% of your body weight can cut knee pain by 50% in many cases. You don’t need to run marathons. Even walking 30 minutes a day, cutting sugary drinks, and eating more vegetables can make a measurable difference in how your joints feel by week six. The goal isn’t perfection—it’s progress. Every pound lost is a pound less grinding on your knees, hips, and lower back.
And it’s not just about pain. Obesity makes arthritis medications less effective. NSAIDs don’t work as well when inflammation is driven by fat tissue. Steroid injections may give temporary relief, but if the source—excess fat—isn’t addressed, the pain comes back faster. That’s why doctors who treat arthritis are now asking about your weight before prescribing anything else. They know the numbers: for every 1-point drop in BMI, there’s a 10% lower risk of needing joint replacement surgery in the next decade.
What you’ll find in these articles isn’t guesswork or hype. It’s real-world data from people who’ve walked out of chronic pain—not by miracle drugs, but by changing how they live. You’ll see how weight loss programs paired with physical therapy beat pills for long-term results. You’ll learn why some arthritis meds work better for certain body types. And you’ll find out what diet and movement patterns actually help, not just what’s trendy.
Osteoarthritis of the Hip: How Weight Loss Can Preserve Your Joint and Reduce Pain
Losing weight can significantly reduce hip pain and slow osteoarthritis progression. Learn how much weight to lose, what diet and exercise work best, and why hip OA responds differently than knee OA.
About
Health and Wellness
Latest Posts

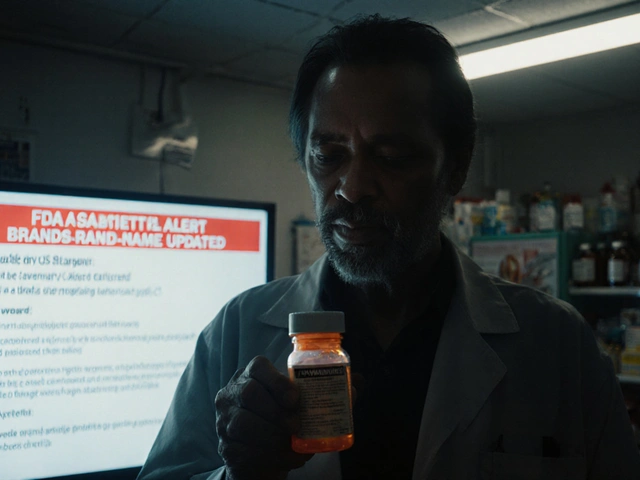
FDA Safety Alerts: Understanding Communications About Generic Drug Problems
By Orion Kingsworth Nov 7, 2025

Steroid Hyperglycemia in Diabetes: How to Adjust Insulin and Medications
By Orion Kingsworth Nov 25, 2025

The Healing Power of Pu-Erh Tea: A Dietary Supplement for a Healthy Mind and Body
By Orion Kingsworth Jul 21, 2023

