Parathyroid Hormone: What It Does, Why It Matters, and How Medications Affect It
When your body needs more parathyroid hormone, a key regulator of calcium levels produced by four small glands in your neck. Also known as PTH, it tells your bones to release calcium, your kidneys to hold onto it, and your gut to absorb more from food. Without it, your muscles cramp, your nerves misfire, and your bones weaken over time. Too much or too little can cause serious problems—like kidney stones from excess calcium, or seizures from dangerously low levels.
This hormone doesn’t work alone. It’s tightly linked to calcium regulation, the body’s constant balancing act to keep blood calcium within a narrow range. When calcium drops, PTH rises. When it’s high, PTH shuts off. But medications can throw this off. Steroids, for example, can raise blood sugar and indirectly mess with calcium balance. Some antibiotics and anticonvulsants alter how your body processes vitamin D, which PTH depends on. Even common painkillers like NSAIDs can affect kidney function, changing how calcium is filtered. And when you switch generic versions of thyroid or calcium supplements, tiny differences in absorption can ripple through your PTH levels—especially if you’re already sensitive.
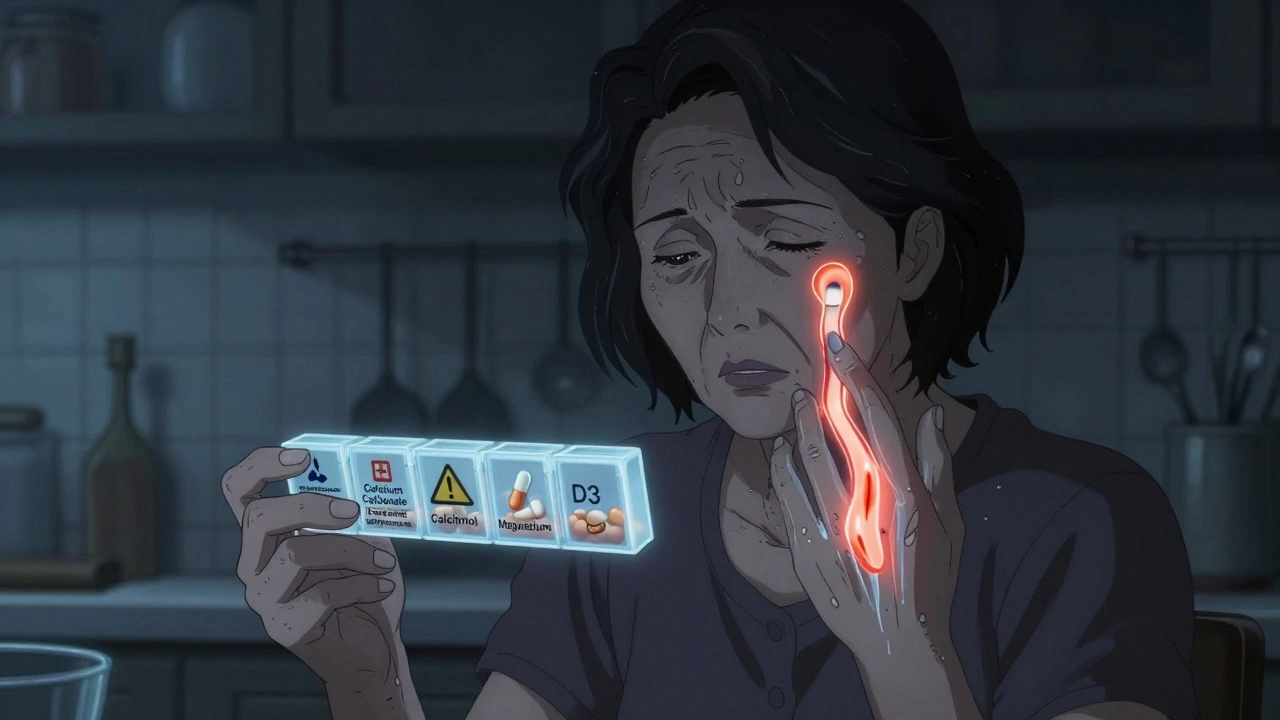
People with hypoparathyroidism, a condition where the glands make too little PTH often need daily calcium and vitamin D pills just to stay stable. Those with hyperparathyroidism, where the glands overproduce PTH, might need surgery or drugs that block bone breakdown. But here’s the catch: many of these treatments interact with other meds. If you’re on diuretics, antacids, or even high-dose vitamin D supplements, your PTH system can get confused. That’s why telling your doctor about every pill, supplement, or herb you take isn’t just good advice—it’s critical. One wrong combo can spike your calcium to dangerous levels or crash it overnight.
Bone health, kidney function, and nerve signaling all hang on this one hormone. That’s why understanding how PTH works—and how your meds influence it—can prevent hospital visits, fractures, and long-term damage. Below, you’ll find real-world stories and data-backed insights on how drug changes, generic switches, and hidden interactions affect people with PTH-related conditions. Whether you’re managing a diagnosed disorder or just wondering why your calcium levels keep bouncing, these posts give you the facts you need to ask the right questions.
Hypoparathyroidism: How to Manage Low Calcium and Vitamin D Effectively
Learn how to manage low calcium and vitamin D in hypoparathyroidism with proven dosing, diet tips, and monitoring strategies to avoid kidney damage and stabilize symptoms long-term.
About
Health and Medicine
Latest Posts


Benzodiazepines and Birth Defect Risks: What Pregnant Women Need to Know
By Orion Kingsworth Feb 7, 2026
Buy Cheap Generic Bactrim Online - Safe Pharmacy Guide 2025
By Orion Kingsworth Sep 30, 2025

Choline Salicylate + Lignocaine for Arthritis Pain: Uses, Safety, Evidence
By Orion Kingsworth Aug 24, 2025