Sedative Interactions: What You Need to Know About Mixing Sleep and Anxiety Meds
When you take a sedative, a medication that slows down brain activity to reduce anxiety, induce sleep, or prevent seizures. Also known as central nervous system depressants, it can seem harmless if taken as directed. But when combined with other drugs—even common ones like alcohol or allergy pills—the results can be life-threatening. Sedatives include prescription drugs like benzodiazepines (Valium, Xanax), sleep aids (Ambien, Lunesta), and even some muscle relaxants. These work by boosting GABA, a brain chemical that calms nerve activity. That’s why they help with anxiety or insomnia. But when another drug does the same thing, your brain can slow down too much.
That’s where drug interactions, when two or more medications affect each other’s effects in the body. Also known as medication clashes, they’re not always obvious. Mixing a sedative with alcohol is the most common mistake. Both depress the nervous system, and together they can cause extreme drowsiness, slow breathing, or even coma. Even OTC sleep aids or antihistamines like diphenhydramine (Benadryl) can act like sedatives. People don’t realize they’re adding fuel to the fire. Then there’s opioids—painkillers like oxycodone or hydrocodone. Combining them with sedatives is one of the leading causes of accidental overdose deaths. The FDA has issued multiple warnings about this combo. And it’s not just pills. Herbal supplements like kava or valerian root can also boost sedative effects. If you’re on any of these, your doctor needs to know—no exceptions.
benzodiazepines, a class of sedatives used for anxiety, seizures, and muscle spasms. Also known as benzos, they’re among the most commonly prescribed but also the most misunderstood. Many patients take them for years without realizing how easily tolerance builds or how dangerous withdrawal can be. And if you’re also taking an antidepressant, a muscle relaxant, or even certain antibiotics like erythromycin, your body may process the benzo slower, leading to buildup. That’s why some people feel foggy or unsteady even on normal doses. The same goes for sleep medications, drugs designed to help you fall or stay asleep. Also known as hypnotics, they’re often prescribed short-term, but people keep taking them. When combined with sedatives for anxiety, the risk of confusion, falls, or memory loss goes up—especially in older adults. And if you’ve ever been told to avoid grapefruit juice with your meds? That applies here too. Grapefruit can interfere with how your liver breaks down many sedatives, making them stronger than intended.
What you’ll find in the posts below aren’t just warnings—they’re real-world examples of how these interactions play out. From people who didn’t tell their doctor about their nightly melatonin to those who ended up in the ER after mixing Xanax with a cold medicine. You’ll learn which combinations are silent killers, what to ask your pharmacist, and how to spot early signs of trouble before it’s too late. This isn’t theory. It’s what happens when people don’t know the risks—and what you can do to stay safe.
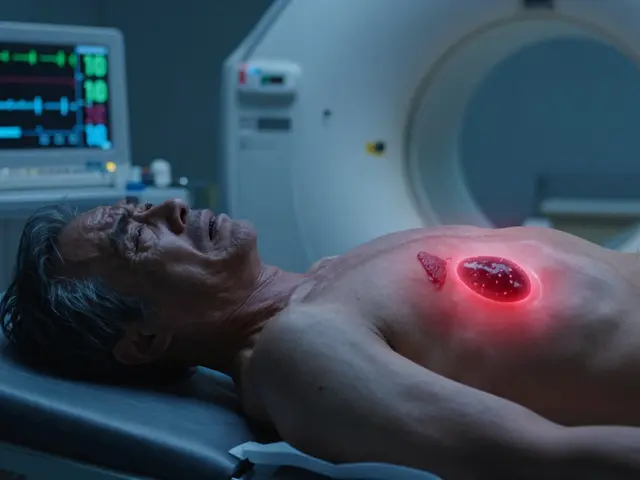
Combining Multiple Sedatives: The Hidden Danger of CNS Depression
Mixing sedatives like opioids, benzodiazepines, and sleep aids can cause deadly respiratory depression. Learn the real risks, who's most vulnerable, and what to do if you're on multiple CNS depressants.
About
Medications
Latest Posts


Top Nolvadex Alternatives in 2025: Your Guide
By Orion Kingsworth Mar 19, 2025
Adrenal Incidentalomas: How to Evaluate and When Surgery Is Needed
By Orion Kingsworth Jan 26, 2026

Itraconazole and its use in combating mold and mildew in homes
By Orion Kingsworth May 13, 2023

