Statin Side Effects: What You Need to Know Before Taking Cholesterol Medication
When you take a statin, a class of drugs used to lower LDL cholesterol and reduce heart attack risk. Also known as HMG-CoA reductase inhibitors, they’re among the most prescribed medications in the world—but not everyone tolerates them well. Millions rely on statins like atorvastatin, rosuvastatin, and simvastatin to keep their arteries clear, but side effects are real, common, and often misunderstood.
One of the most frequent complaints? muscle pain, a dull ache or weakness that can start weeks after beginning treatment. It’s not always serious, but if it’s constant, worsening, or paired with dark urine, it could be rhabdomyolysis—a rare but dangerous breakdown of muscle tissue. Most people feel mild soreness that fades, but if it stops you from walking or lifting, talk to your doctor. You might need a lower dose, a different statin, or a non-statin alternative like ezetimibe.
Another hidden issue? liver enzyme changes, elevated ALT or AST levels detected in routine blood tests. This doesn’t mean your liver is damaged—it just means the statin is being processed. Most cases stay mild and don’t require stopping the drug. But if levels jump above three times the normal range, your doctor will likely pause treatment and retest. It’s not a reason to panic, but it’s a reason to get tested regularly.
Then there’s the less talked about stuff: blood sugar changes, a slight rise in HbA1c that may increase diabetes risk in predisposed people. Studies show statins slightly raise fasting glucose, but the heart protection they offer still outweighs the risk for most. Still, if you’re prediabetic, your doctor should monitor your levels more closely.
Some people report brain fog, memory lapses, or trouble sleeping. The science here is mixed—some studies link statins to these symptoms, others don’t. But if you notice a change after starting a statin, track it. Write down when it started, how often it happens, and whether it improves after stopping the drug. That info helps your doctor decide if it’s the statin or something else.
And don’t forget drug interactions. Statins can react badly with certain antibiotics, antifungals, grapefruit juice, and even some supplements like red yeast rice. These can spike statin levels in your blood and make side effects worse. Always tell your pharmacist and doctor what else you’re taking—even if it’s "just a natural remedy."
What’s Next? You’re Not Alone
There’s no one-size-fits-all when it comes to statins. What works for your neighbor might cause you serious discomfort. The posts below cover real cases—people who switched from Crestor to pravastatin and felt better, others who managed muscle pain with CoQ10, and how to tell if your symptoms are normal or a red flag. You’ll find practical advice on monitoring, alternatives, and how to talk to your doctor without sounding like you’re doubting the treatment. This isn’t about avoiding statins—it’s about using them safely, smartly, and with your full awareness.
Muscle Aches from Statins: What Really Causes It and What to Do
Muscle pain from statins is common but often misunderstood. Learn what's really causing it, how to tell if it's serious, and what to do next without risking your heart health.
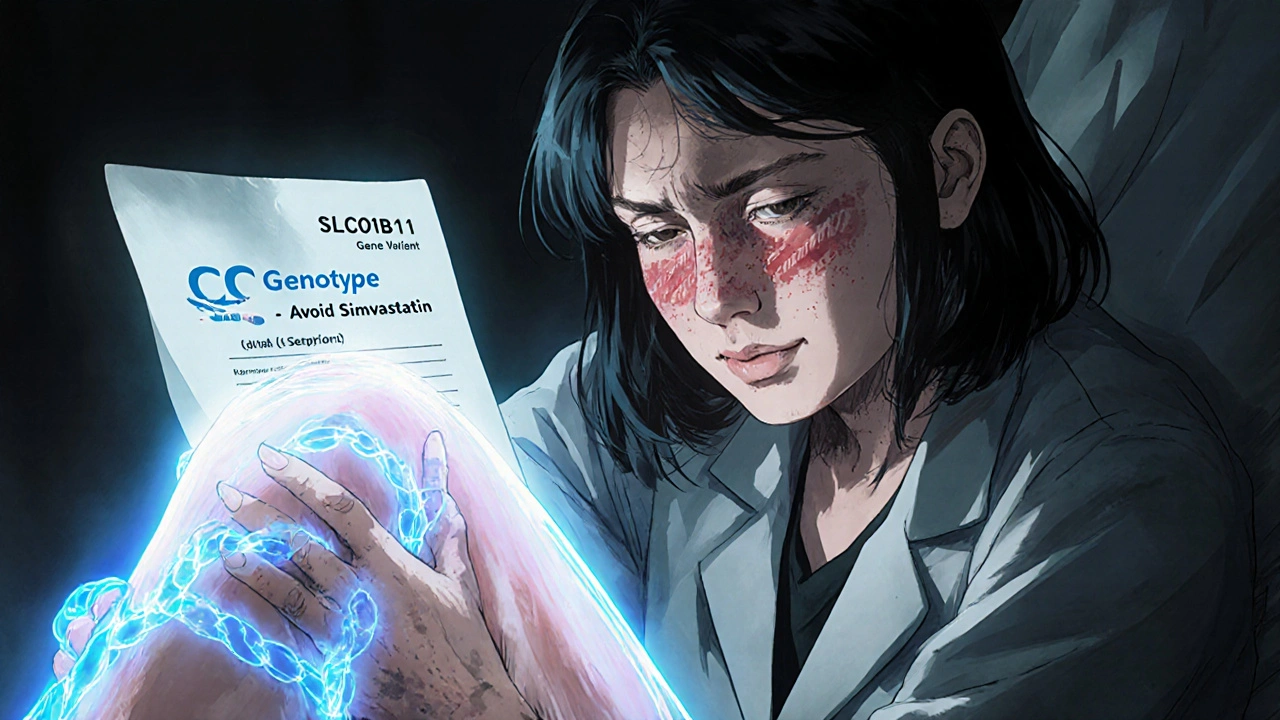
Genetic Factors in Statin Tolerance: How Pharmacogenomics Testing Can Help You Stay on Your Medication
Discover how genetic testing can reveal why some people can't tolerate statins-and how to find a safer alternative based on your DNA. Learn about SLCO1B1, statin choices, insurance coverage, and real-world success stories.
About
Medications
Latest Posts


Wild Thyme vs Common Thyme: Essential Oil Potency, Chemotype Differences, and Health Benefits Unveiled
By Orion Kingsworth Apr 30, 2025

Unlock the Healing Potential of German Chamomile: Your Ultimate Guide
By Orion Kingsworth May 10, 2024

How to Read OTC Drug Facts Labels Correctly and Confidently
By Orion Kingsworth Jan 26, 2026