Taking medication every day for years isn’t just routine-it’s life-saving. But it’s also risky. If you’re managing diabetes, high blood pressure, arthritis, or heart disease, you’re likely on multiple drugs. And the longer you take them, the more dangerous mistakes can become. Medication safety isn’t about remembering to take your pills. It’s about understanding how they work together, spotting hidden dangers, and staying in control-even when life gets messy.
Why Long-Term Medication Use Is a Hidden Risk
Most people think if a doctor prescribed it, it’s safe. But that’s not true over time. When you’re on five or more medications-a common situation for adults over 65-your risk of bad reactions jumps dramatically. Studies show nearly 91% of people in long-term care take at least five drugs daily. That’s not normal. That’s a ticking clock.
Each extra pill adds a new chance for side effects, interactions, or confusion. A painkiller like diclofenac might be fine alone. But add it to aspirin or a blood thinner, and you’re looking at stomach bleeding. A sleep aid might help tonight, but if you’ve been on it for months, your brain forgets how to rest without it. These aren’t rare mistakes. They’re systemic.
The CDC estimates that medication non-adherence causes about 125,000 deaths in the U.S. every year. That’s more than car crashes. And it’s not because people are careless. It’s because the system doesn’t help them stay safe.
Your Medication List: Your Most Important Document
Every time you see a doctor, pharmacist, or go to the ER, you need one thing: an up-to-date list of everything you take. Not just prescriptions. Not just the big ones. Everything.
That includes:
- Brand and generic names
- Dosage (e.g., 10 mg, 2 tablets)
- How often (e.g., once daily, every 8 hours)
- Why you take it (e.g., “for blood pressure,” “for joint pain”)
- When you last refilled it
- Any over-the-counter drugs, vitamins, or supplements
Don’t rely on memory. Don’t trust your pill organizer. Write it down. Keep it in your wallet. Save it on your phone. Update it every time something changes-even if it’s just a new bottle from the pharmacy.
Why? Because when you’re rushed, confused, or in pain, no one will know what you’re taking unless you show them. And if they guess wrong, it could kill you.
The 7 Rights of Safe Medication Use
Healthcare workers use a checklist called the “7 Rights” to avoid mistakes. You should use it too.
- Right patient - Is this medicine really for you? Check your name on the bottle.
- Right drug - Does the name match your list? Don’t assume the color or shape means it’s the same.
- Right dose - Is it the same as your doctor said? A 5 mg tablet isn’t the same as a 10 mg one.
- Right route - Is it meant to be swallowed, injected, or applied to the skin? Never crush pills unless told it’s safe.
- Right time - Are you taking it with food? At night? Every 12 hours? Timing matters.
- Right documentation - Did you write down when you took it? Use a simple log or app.
- Right reason and response - Why are you taking this? And what should you feel? If you feel dizzy, nauseous, or confused, write it down and tell your doctor.
These aren’t just rules for nurses. They’re your shield.
Polypharmacy: When More Isn’t Better
Polypharmacy isn’t a dirty word. It’s a reality for millions. But it’s not harmless. The American Academy of Family Physicians says taking five or more medications increases your risk of falls, confusion, hospital stays, and even death.
Here’s the problem: You might see a cardiologist, a rheumatologist, a neurologist, and a primary care doctor-all prescribing drugs. No one is looking at the whole picture. That’s why you need a medication review at least once a year.
Ask your doctor: “Is every pill I’m taking still necessary?”
Some medications lose their benefit after months or years. A sleep aid you started five years ago might not help anymore-but you’re still taking it because no one asked you to stop. A painkiller you got after surgery might be causing stomach damage now. A statin you were put on for cholesterol might be doing more harm than good if your numbers are now normal.
Don’t be afraid to ask. Your doctor should welcome the question.
How to Spot Side Effects Before They Hurt You
Side effects don’t always show up right away. Sometimes they creep in slowly. You might think, “I’m just getting older,” or “I’m tired because I’m stressed.” But it could be your meds.
Watch for these red flags:
- Sudden dizziness or balance problems
- Memory lapses or confusion
- Unexplained bruising or bleeding
- Swelling in ankles or feet
- Loss of appetite or weight loss
- Constipation or diarrhea that won’t go away
- Feeling unusually sleepy or wired
Keep a simple journal. Write down: “Date,” “Medicine,” “How I felt.” After a few weeks, patterns emerge. You might notice every time you take your blood pressure pill in the evening, you wake up dizzy. That’s not normal. That’s a signal.
Bring your journal to your next appointment. It’s the most powerful tool you have.
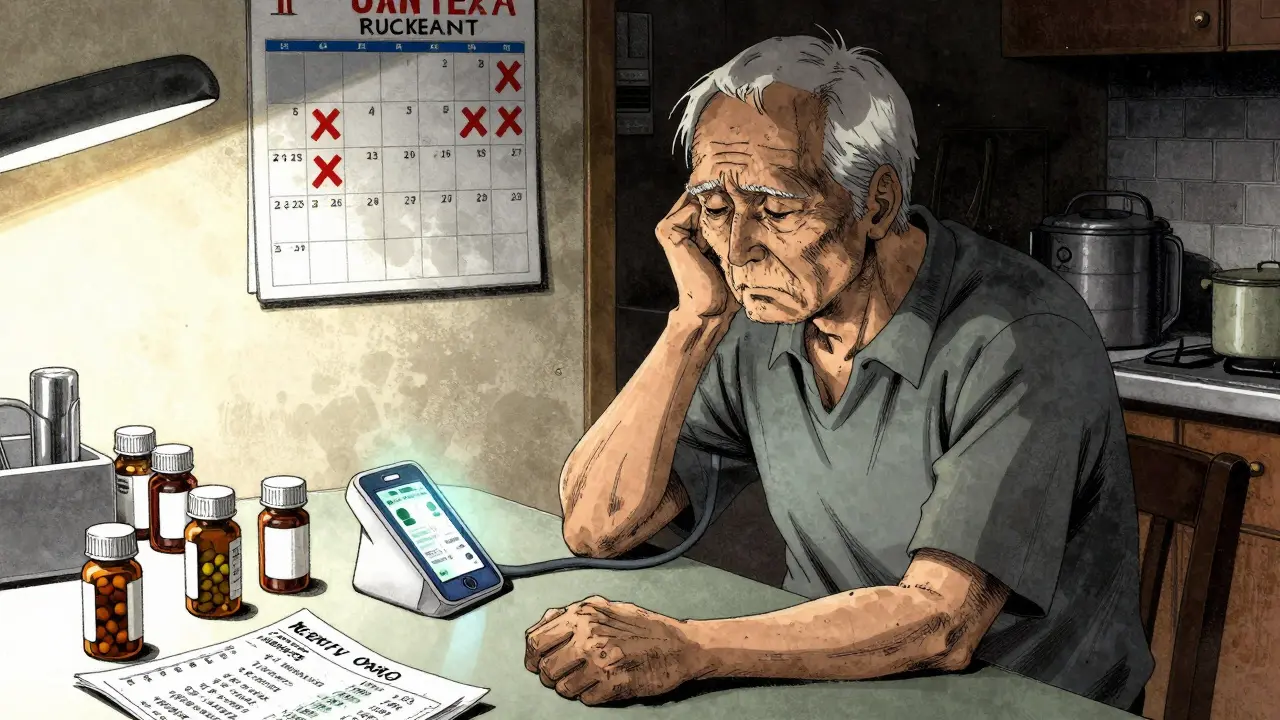
Technology Can Help-If You Use It Right
You don’t need fancy gadgets. But you do need simple tech to stay safe.
- Pill dispensers with alarms - They beep when it’s time, and some even lock until the right hour.
- Medication apps - Apps like Medisafe or MyTherapy track doses, send reminders, and can alert your family if you miss a dose.
- Electronic health records - Ask your doctor if your prescriptions are synced across providers. If not, push for it.
- Pharmacy alerts - Many pharmacies now flag dangerous drug interactions when you pick up a new prescription. Make sure yours does.
One study found that using tech tools reduced medication errors by 55% in older adults. That’s not magic. That’s math.
Who Can Help You Stay Safe?
You don’t have to do this alone. Your pharmacist is your best ally.
Pharmacists don’t just hand out pills. They know how drugs interact. They know which ones are outdated. They can spot if you’re taking two drugs that should never be mixed.
Ask your pharmacist: “Can you review all my medications once a year?” Most will do it for free. Bring your list. Ask them to check for duplicates, unnecessary drugs, or risks.
Also, look into a Medication Therapy Management (MTM) program. These are free services offered by many Medicare Part D plans. A pharmacist spends 30 minutes with you, reviews everything, and gives you a written action plan. You can find one by calling your plan’s customer service.

Cost Shouldn’t Stop You From Being Safe
One in four Americans skips doses because they can’t afford their meds. That’s not just risky-it’s deadly.
But you have options:
- Ask for generics. They’re the same drug, cheaper.
- Use mail-order pharmacies. Many offer 90-day supplies at lower prices.
- Check patient assistance programs. Drugmakers often give free or low-cost meds to those who qualify.
- Ask your doctor if you can switch to a cheaper alternative.
Never cut pills in half unless your doctor says it’s safe. Never stop a drug because it’s expensive. Talk to someone. There’s always a way.
What to Do When You’re Not Sure
You’re not supposed to know everything. That’s why you have a team.
If you’re confused about a new prescription, say: “Can you explain this again? I want to make sure I understand.”
If you feel worse after starting a new drug, call your doctor. Don’t wait. Don’t assume it’ll pass.
If you’re not sure if you took your pill, don’t guess. Don’t double up. Wait until the next scheduled time.
And if you ever feel like you’re drowning in pills-say it. Your health isn’t about how many drugs you take. It’s about how well you live with them.
How often should I review my medications with my doctor?
At least once a year, or anytime you see a new specialist, start a new medication, or notice side effects. If you’re on five or more drugs, ask for a formal medication review. Some clinics offer this as a standard part of your annual check-up.
Can I stop a medication if I feel fine?
Never stop a prescribed medication without talking to your doctor-even if you feel great. Some drugs, like blood pressure or antidepressants, need to be tapered slowly. Stopping suddenly can cause rebound effects, dangerous spikes, or withdrawal symptoms. Always ask first.
What should I do if I miss a dose?
Check the label or ask your pharmacist. For most medications, if you miss a dose by a few hours, take it as soon as you remember. If it’s almost time for the next dose, skip the missed one. Never double up unless told to. If you’re unsure, call your pharmacy. They’re trained to help.
Are over-the-counter drugs safe to take with my prescriptions?
Not always. Common OTC drugs like ibuprofen, antacids, or sleep aids can interact badly with blood pressure meds, blood thinners, or antidepressants. Always tell your pharmacist or doctor about every OTC product you use-even if you think it’s harmless.
How can I tell if a medication is no longer needed?
Ask your doctor: “Is this still helping me?” Some meds are meant for short-term use but become long-term by accident. For example, a painkiller after surgery, a sleep aid after stress, or a cholesterol drug if your levels improved. A medication review can help identify drugs that are no longer necessary or safe.
Final Thought: Safety Is a Habit, Not a One-Time Fix
Medication safety isn’t something you do once a year at your check-up. It’s daily. It’s writing down what you take. It’s asking questions. It’s saying no to a new pill until you understand why. It’s knowing your pharmacist’s name and calling them when you’re unsure.
Chronic illness doesn’t mean giving up control. It means taking it back-bit by bit, pill by pill.



beth cordell
January 12, 2026 at 09:20
I literally keep my med list on my phone lock screen 📱💊 and my pharmacist knows me by name. Also, I use Medisafe and it beeps like a tiny angel telling me to take my pills. No more guessing!