Drug Manufacturing: How Medicines Are Made and Why It Matters for Your Health
When you pick up a pill at the pharmacy, you’re holding the result of drug manufacturing, the complex process of creating medications from raw chemicals to finished tablets or injections. Also known as pharmaceutical production, it’s not just mixing powders—it’s precision science, strict controls, and global supply chains that determine whether your medicine works—or puts you at risk. Every tablet, capsule, or injection you take started as a chemical compound, often made in a factory thousands of miles away. The difference between a safe drug and a dangerous one isn’t just the active ingredient—it’s how it was made, tested, and inspected.
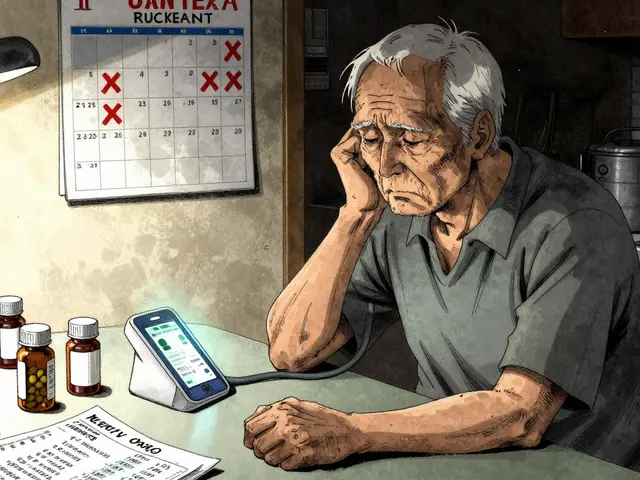
Generic drugs, affordable copies of brand-name medications, make up most of what’s on pharmacy shelves today. But not all generics are created equal. Some are made in facilities with poor quality controls, leading to recalls over contamination like nitrosamines, cancer-causing impurities found in blood pressure and diabetes meds. Others fail because they don’t dissolve the same way as the original, causing therapeutic failure, when a generic doesn’t work as expected despite meeting regulatory standards. Even API manufacturing, the production of the active pharmaceutical ingredient, often happens overseas, with China supplying 80% of the world’s raw drug components. FDA inspections have found widespread issues: falsified data, dirty equipment, and missing safety checks. That’s why a drug approved by the FDA doesn’t always mean it’s safe—it means it passed a checklist, not a guarantee of perfection.
What you’re seeing in the news—recalls, safety alerts, lawsuits over contaminated meds—isn’t random. It’s the result of a system under pressure. Companies cut corners to save money. Regulators are stretched thin. And patients? They’re left guessing whether their medicine is reliable. But you don’t have to be in the dark. The posts below break down real cases: how a generic failed a diabetic patient, why a Chinese-made batch triggered a nationwide recall, how authorized generics are actually identical to brand-name drugs, and what the FDA does (and doesn’t do) to catch dangerous products. You’ll see how weight loss affects drug metabolism, how genetic differences change how your body handles statins, and why a simple inhaler cleaning mistake can put your life at risk. This isn’t theory. It’s what’s happening in your medicine cabinet right now.
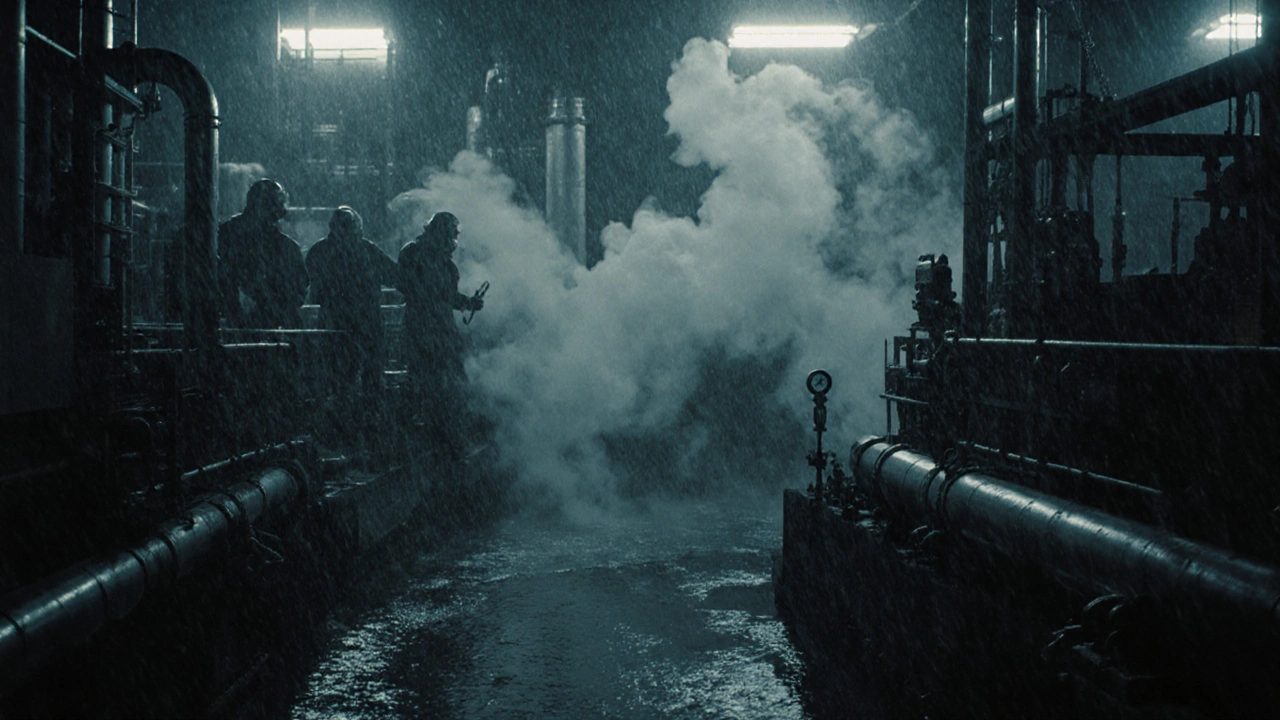
The Environmental Impact of Eflornithine Production
Eflornithine saves lives from sleeping sickness, but its chemical production generates toxic waste and high emissions. A greener method exists - but isn't being used. Here's why.
About
Medications
Latest Posts

Ramipril (Altace) vs. Common Alternatives - Full Comparison
By Orion Kingsworth Oct 10, 2025
Medication Safety for Chronic Conditions: Essential Long-Term Use Tips
By Orion Kingsworth Jan 11, 2026

OpenFDA API vs FAERS: How to Pull Side‑Effect Reports and Detect Signals
By Orion Kingsworth Oct 26, 2025