Opioid and Benzodiazepine Risks: What You Need to Know
When you take opioids, powerful pain relievers like oxycodone, hydrocodone, or morphine that slow breathing and reduce pain signals and benzodiazepines, sedatives like diazepam, alprazolam, or lorazepam used for anxiety, insomnia, or seizures at the same time, you’re doubling down on a danger that kills thousands every year. These drugs don’t just add up—they multiply. Both slow your breathing, and together, they can shut it down completely. The CDC says more than 30% of opioid overdose deaths involve benzodiazepines. It’s not a rare mistake. It’s a common, preventable tragedy.
Why does this happen? Opioids act on brainstem receptors that control breathing. Benzodiazepines boost the effect of GABA, a calming neurotransmitter that also suppresses respiratory drive. When you mix them, your brain gets the message to breathe slower… and slower… until it stops. No warning. No second chance. Even people who’ve taken either drug for years without issue can suddenly crash when the other is added—even at low doses. Doctors know this. That’s why guidelines now say: avoid combining them unless absolutely necessary, and never without close monitoring.
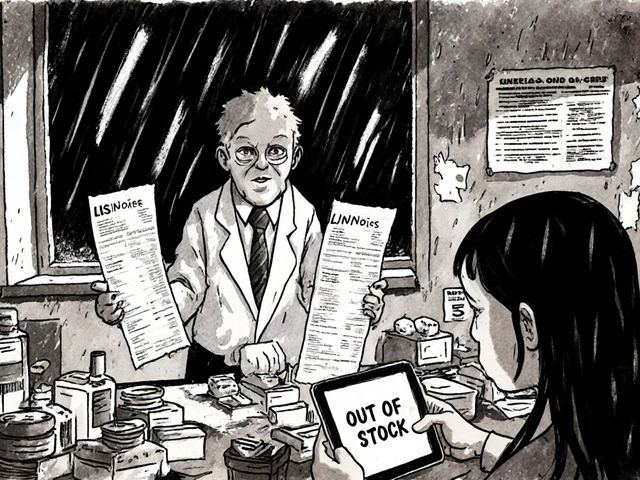
It’s not just about overdoses. Long-term use of either drug leads to dependence. Withdrawal from opioids is brutal—nausea, cramps, sweating. Withdrawal from benzodiazepines? Seizures, hallucinations, even death if stopped cold. Many people start one for pain, then the other for anxiety caused by the pain, then another for the insomnia caused by both. It spirals fast. And because these drugs are often prescribed by different doctors, patients rarely realize they’re stacking risks. You might think your sleep aid is harmless, or your painkiller is just a quick fix. But together, they’re a silent timer.
What can you do? If you’re on either, ask your doctor if you really need both. Can you try non-drug options for anxiety—therapy, exercise, mindfulness? For pain, can physical therapy or nerve blocks help? If you’re already on both, don’t quit cold turkey. Talk to your provider about a slow, safe taper. Keep a list of every medication and supplement you take—write it down, bring it to every appointment. And if you live alone, tell someone you trust what you’re taking. They might be the one who calls 911 if you stop breathing.
Below, you’ll find real-world advice from people who’ve been there—how to spot early signs of trouble, what alternatives actually work, and how to talk to your doctor without sounding alarmist. These aren’t theoretical warnings. These are lessons learned the hard way. And they could save your life.
Combining Multiple Sedatives: The Hidden Danger of CNS Depression
Mixing sedatives like opioids, benzodiazepines, and sleep aids can cause deadly respiratory depression. Learn the real risks, who's most vulnerable, and what to do if you're on multiple CNS depressants.
About
Medications
Latest Posts

Lymphoma in the Aging Population: Key Challenges & Practical Considerations
By Orion Kingsworth Sep 22, 2025

Amlodipine and POTS Syndrome: Can This Medication Help with Symptoms?
By Orion Kingsworth Apr 28, 2023

The Relationship Between Bisoprolol Fumarate and Anxiety
By Orion Kingsworth Apr 27, 2023

