Pharmacy Benefit Managers: How They Control Your Drug Costs and What It Means for You
When you pick up a prescription, pharmacy benefit managers, third-party administrators that negotiate drug prices and manage prescription benefits for insurers. Also known as PBMs, they sit between drug makers, pharmacies, and your health plan — and they decide what medications are covered and at what price. Most people don’t realize PBMs control over 80% of prescription drug spending in the U.S. They don’t make drugs. They don’t dispense them. But they hold the keys to whether your medicine is affordable — or even available.
How do they do it? Through formularies, lists of approved drugs that insurers will pay for. If your drug isn’t on the list, you pay full price — or nothing at all. PBMs push cheaper generic drugs, lower-cost versions of brand-name medications with the same active ingredients because they earn rebates from manufacturers who want to be on those lists. That’s why your doctor might switch your brand-name statin to a generic — not because it’s better, but because the PBM gets paid more when you take it. But here’s the catch: sometimes the generic they push isn’t the one that works for you. We’ve seen cases where switching generics caused therapeutic failures, especially with drugs that have a narrow therapeutic index. And when PBMs restrict access to a drug you rely on, it’s not just an inconvenience — it can be dangerous.
PBMs also control which pharmacies you can use. If your local pharmacy isn’t in their network, you’ll pay more — or be forced to mail-order your meds. And when drug shortages hit, PBMs decide which alternatives get priority. That’s why some patients can’t get their usual antibiotic or insulin, even when it’s in stock elsewhere. The system isn’t broken — it’s designed this way. PBMs profit from complexity. They hide rebates, shift costs to patients, and change formularies without warning. You might think your insurance covers your meds, but if the PBM says no, your coverage doesn’t matter.
The posts below dig into the real-world effects of this system. You’ll find stories about how pharmacy benefit managers influence generic drug choices, why some medications get pulled from formularies overnight, and how patients fight back when their treatment gets blocked. You’ll see how drug shortages, pricing tricks, and insurer rules all tie back to PBMs. Whether you’re managing a chronic condition, juggling multiple meds, or just trying to afford your prescriptions, understanding how these middlemen operate isn’t optional — it’s essential. What you learn here could save you money, time, and even your health.
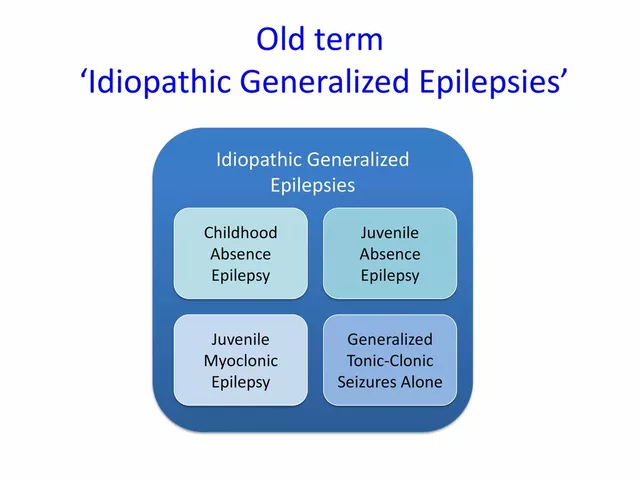
Insurance Benefit Design: How Health Plans Use Generics to Cut Costs
Health plans use tiered formularies, mandatory substitutions, and step therapy to push patients toward generic drugs-saving billions while cutting patient costs. But hidden pricing practices can leave you paying more than you should.
About
Medications
Latest Posts

Natural vs. Synthetic Calcium Carbonate: What's The Difference?
By Orion Kingsworth Feb 5, 2025

Amoxicillin for Tonsillitis: Dosage, Effectiveness, and Side Effects
By Orion Kingsworth May 29, 2023

OpenFDA API vs FAERS: How to Pull Side‑Effect Reports and Detect Signals
By Orion Kingsworth Oct 26, 2025