Vitamin D: What It Does, Who Needs It, and What You Should Know
When you think of vitamin D, a fat-soluble nutrient your skin makes when exposed to sunlight, essential for calcium absorption and immune function. Also known as the sunshine vitamin, it’s not really a vitamin at all—it’s a hormone your body produces to keep bones strong, muscles working, and your immune system alert. Most people don’t get enough, even in sunny places. Why? We stay indoors, wear sunscreen, live in cities with tall buildings, or have darker skin that blocks UV rays more efficiently. The result? Low levels are one of the most common nutrient deficiencies worldwide.
Vitamin D deficiency, a condition where your body lacks sufficient vitamin D to support bone health and immune response doesn’t always cause obvious symptoms. But over time, it can lead to weak bones, muscle pain, fatigue, and even increased risk of infections. People over 65, those with obesity, people with dark skin, and anyone who doesn’t get outside much are at higher risk. Even if you eat fish, eggs, or fortified milk, it’s often not enough—your body needs sunlight or a supplement to hit target levels.
Vitamin D supplements, oral forms of vitamin D, typically D2 or D3, used to correct deficiency or maintain healthy levels when sun exposure is limited are common, but not all are equal. D3 (cholecalciferol) is the form your body naturally makes and uses best. D2 (ergocalciferol), often found in plant-based supplements, is less effective at raising blood levels. Taking too much can be dangerous—excess vitamin D causes calcium to build up in your blood, which can harm your kidneys and heart. Most adults need 600–800 IU daily, but if you’re deficient, your doctor might recommend 1,000–4,000 IU for a few months to catch up.
It’s not just about bones. Research shows vitamin D plays a role in regulating mood, reducing inflammation, and helping your immune system fight off viruses. Low levels have been linked to seasonal depression, autoimmune conditions, and even slower recovery from illness. But taking mega-doses won’t make you invincible. The goal isn’t to overdo it—it’s to get to a healthy baseline.
Here’s what you’ll find in the posts below: how vitamin D interacts with other medications, why some people still get deficient even when taking supplements, what blood tests actually tell you, and how conditions like GERD, diabetes, or steroid use can mess with your vitamin D levels. You’ll also see real cases where supplement use clashed with other drugs—like when herbal remedies or antibiotics changed how your body handled it. No fluff. Just what works, what doesn’t, and what your doctor might not tell you.
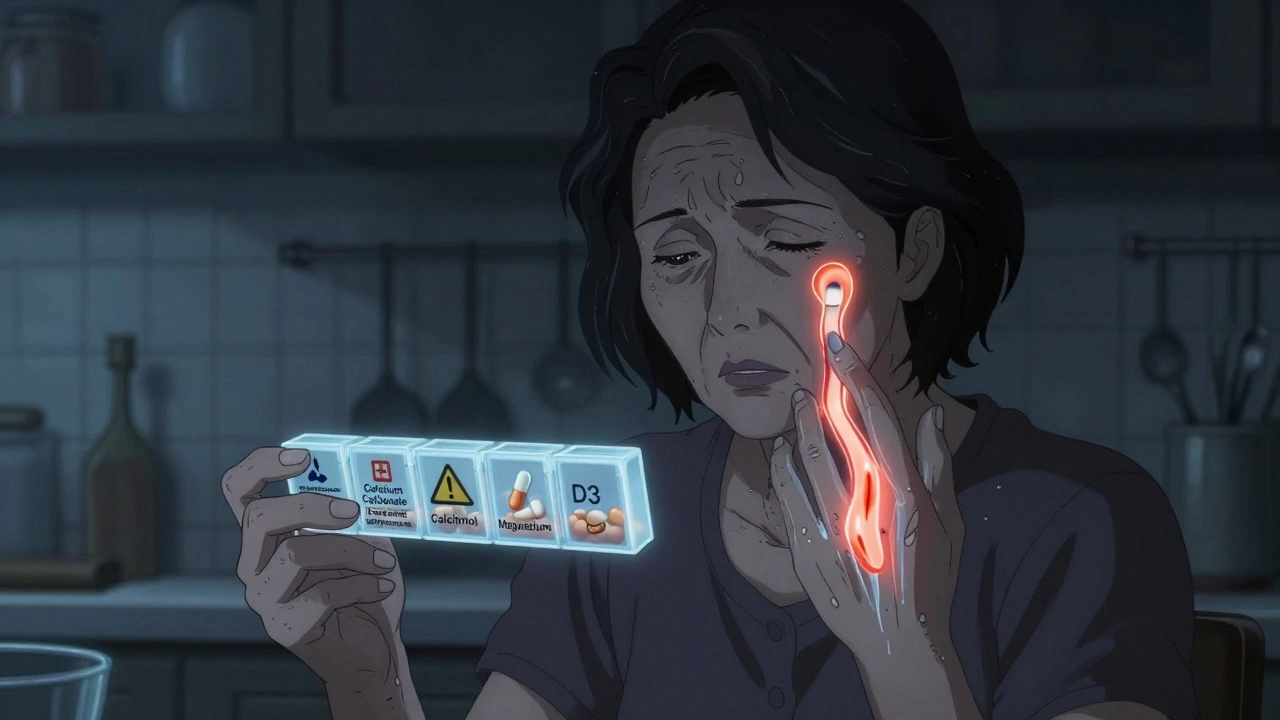
Hypoparathyroidism: How to Manage Low Calcium and Vitamin D Effectively
Learn how to manage low calcium and vitamin D in hypoparathyroidism with proven dosing, diet tips, and monitoring strategies to avoid kidney damage and stabilize symptoms long-term.
About
Health and Medicine
Latest Posts


Amoxicillin for Tonsillitis: Dosage, Effectiveness, and Side Effects
By Orion Kingsworth May 29, 2023
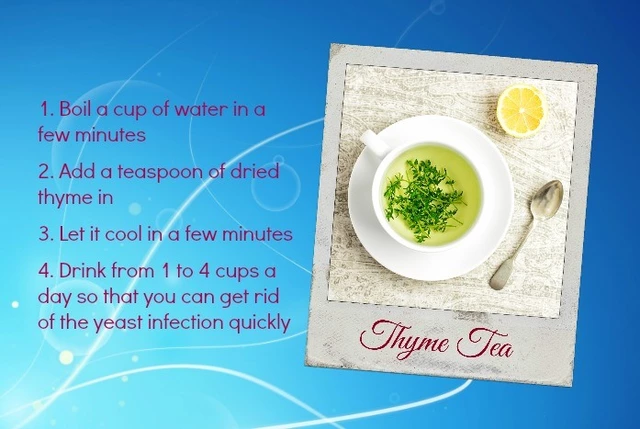
Home Remedies for Yeast Infections of the Skin: What Works and What Doesn't
By Orion Kingsworth May 6, 2023

Exploring the Best Alternatives to Propecia for Hair Loss in 2024
By Orion Kingsworth Oct 19, 2024